Assessment of the Association of Social Isolation Measures in the COVID-19 Pandemic with Exacerbations in Chronic Lung Disease
Flavia Velasco Fernandes*
Department of Human Resource and Management Analytics, Indian Institute of Management Kozhikode, Maharashtra, India
- *Corresponding Author:
- Flavia Velasco Fernandes
Department of Human Resource and Management Analytics,
Indian Institute of Management Kozhikode,
Maharashtra,
India;
E-mail: fcvelasco@hotmail.com
Received date: October 17, 2022, Manuscript No. IPJL-22-14811; Editor assigned date: October 19, 2022, PreQC No. IPJL-22-14811(PQ); Reviewed date: November 02, 2022, QC No. IPJL-22-14811; Revised date: January 05, 2023, Manuscript No. IPJL-22-14811(R); Published date: January 12, 2023, DOI: 10.36648/IPJL.4.1.001
Citation: Fernandes FV (2023) Assessment of the Association of Social Isolation Measures in the COVID-19 Pandemic with Exacerbations in Chronic Lung Disease. J Lung Vol:4 No:1
Abstract
Objective: To evaluate the association between social isolation and frequency of exacerbations in patients with chronic lung disease.
Methods: This observational, descriptive, cross-sectional study included patients scheduled for pulmonology outpatient clinic appointments from March to July 2020, when outpatient appointments were suspended due to the COVID-19 pandemic. A questionnaire survey was conducted using recorded telephone calls.
Results: Overall, 516 patients were scheduled for outpatient appointments during the study period. Of these, 344 patients were excluded due to access issues or refusal to participate. In the 172 included patients, asthma and COPD were most prevalent (40.1% and 25.6%, respectively). Most people left homeless often after isolation commenced (93%) and had no difficulty in obtaining medications (80.2%). No exacerbations occurred in 117 patients (68%) during this period. Exacerbation was associated with patients who consulted a physician (27.3%, p=0.01), who considered themselves unwell (69.1%, p<0.01) and who had severe dyspnea levels (grade 2-3 and 4-5: 61.8% and 18.2%, respectively; p<0.01). Exacerbation absence was associated with the lowest dyspnea severity (grade 0-1: 52.1%, p<0.01). In terms of sociodemographics, lifestyle habits and risk factors, exacerbation was only associated with Black patients (21.8%, p=0.04).
Conclusions: Remaining home was associated with reduced chronic lung disease exacerbations, whereas exacerbations occurred in those who sought medical care, reported worse symptoms, considered themselves unwell or were Black. This underscores the need for the use of masks, hand hygiene, virus control measures to reduce lung disease exacerbations.
Keywords
Lung diseases; Social isolation; Symptom flare up; Hand hygiene
Introduction
In late 2019, the emergence of the new coronavirus SARSCoV- 2 caused a series of pneumonia cases in the city of Wuhan, China, which spread exponentially. The disease, COVID-19, was declared a pandemic by the world health organization on March 11, 2020 [1-3].
Since SARS-CoV-2 is a highly transmissible virus, the Ministry of Health in Brazil, as of March 2020, instituted several measures of social isolation, social distancing, hand hygiene and use of masks in order to curb the transmission of the virus, flatten the epidemiological curve and reduce the number of hospitalizations. XXX hospital, in accordance with national recommendations and state ordinances, determined that all outpatient clinics, including pulmonology clinics, should be suspended during that period [4-6].
Despite the importance of social isolation measures, this raised a concern about the influence of these measures on the care of patients with chronic diseases, particularly among the Brazilian unified health system users [7]. Another concern was that the lack of scheduled appointments would somehow impair the follow-up of patients with chronic lung diseases or even that exacerbations, typically identified and treated in basic health care units, would become a problem, as emergency health care units were overloaded with patients diagnosed with COVID-19 [8].
People with chronic lung diseases need regular outpatient medical monitoring to evaluate whether the underlying disease is under control, adherence to clinical treatment, renewal of prescriptions for chronic medications and treatment of any exacerbations of the clinical condition. These patients develop exacerbations when in contact with viruses, bacteria, allergens or with inadequate use of medications, which can lead to severe decompensation and even death [9].
It has been reported that isolation measures worldwide led to a reduction in the transmission of SARS-CoV-2 and other viruses, which may be associated with a reduction in exacerbation of chronic lung diseases [10-12]. There is little evidence indicating that patients with chronic lung diseases are more susceptible to or develop more severe SARS-CoV-2 infection than do those without these diseases [13,14]. In fact, numerous studies report a reduction in exacerbations of chronic lung disease and in healthcare use by these patients during the pandemic [15-17].
Against this background, it is of great importance to investigate and describe the conditions of isolation during the COVID-19 pandemic, to identify which factors might be associated with exacerbation of chronic lung disease during this period and to ascertain how social isolation measures influenced this.
Materials and Methods
The ethics committee of the XXX hospital, approved this study (CEP/CONEP, 13/05/2020; favorable opinion 127 [1328452]).
This was an observational, cross-sectional and descriptive study, in which patients who were followed up in the pulmonology outpatient clinics of XXX Hospital were evaluated. We evaluated patients who were scheduled for appointments between March 19, 2020 and July 31, 2020, at the Chronic Obstructive Pulmonary Disease (COPD), asthma, pulmonary circulation, cystic fibrosis and bronchiectasis outpatient clinics of XXX hospital. During this period, elective outpatient appointments were suspended, in compliance with the social isolation measures set out by the ministry of health during the COVID-19 pandemic.
The patients were contacted by telephone and invited to participate in the research in the period from April to July 2020. The calls were made and recorded using the researcher's personal cellular phone. Patients were informed of the research objectives and the Informed Consent Form (ICF) used and were invited to participate in the study. Patients who agreed to participate as recorded on the call and who met the inclusion criteria, answered the questions asked by the researcher over the phone. Patients who did not agree to the ICF or who were unable to access the telephone or answer the research questionnaires were excluded from the study.
Variables collected
The data collection instrument was prepared by pulmonologists from the institution (Appendix 1). The form was filled out over the telephone by the researcher, while the call was recorded. The data obtained included epidemiological evaluation, isolation characteristics, access to medication, flareups during the period and perception of symptoms. For the latter, the patient reported a score ranging from 0 to 5 (0: no symptoms, 5: the worst symptoms). An exacerbation was considered if the patient answered yes to at least one of the following questions: Flare-ups in the last 3 months due to respiratory problems; sought emergency care or changed some medication due to respiratory problems; required hospitalization (more than 24 hours) due to respiratory problems.
As risk factors for exacerbations, we considered the following: participants, who left home more, stopped doing physical activity, lacked clarification of doubts about the disease and did not adhere or have access to medication. Among these, we analyzed isolation at home (worked outside the home, left homeless after the beginning of isolation, needed help with shopping/needs outside the home, went beyond the limits of the home), access to and use of medications (used the medications as prescribed, had difficulty in obtaining medications, had access to medications at the High-Cost Medication Center (CMAC), physical activities (stopped practicing physical activities during isolation) and medical doubts and clarifications (clarified uncertainties with a doctor, had uncertainties/fear in relation to medications, some uncertainties were not clarified).
After the end of the call, each recording was sent to a Google Drive database, where it was stored.
Statistical analysis
Data were recorded in a Microsoft Excel spreadsheet and analyzed with the help of SPSS software. Patients' sociodemographic profile and lifestyle habits were characterized using absolute frequency (n) and relative frequency (%). The distribution of the profile of patients according to the occurrence of exacerbations was tested using Pearson's chi-square with post-hoc tests as described by MacDonald and Gardner. The level of significance adopted was 5% (p<0.05) [18].
Results
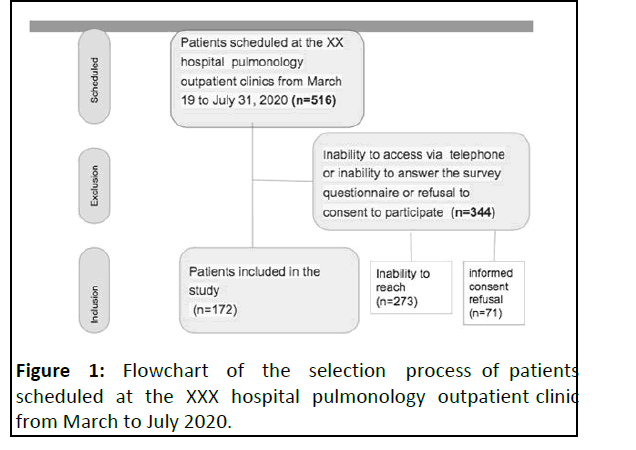
During the period evaluated, 516 patients were scheduled for appointments at XXX hospital pulmonology outpatient clinics. A total of 344 patients were excluded due to inability to access them by telephone, their inability to answer the survey questionnaires or their refusal to participate in the survey. Thus, 172 patients were included in the study (Figure 1).
In terms of the sociodemographic profile, most patients were over 60 years old (43%), were female (73.8%), were of mixed race (48.3%) and lived in the metropolitan area of Goiania (70.3%). The most prevalent family income was 1-3 minimum wages (51.2%) and most participants reported having had elementary school education (54.1%). Most obtained news about the pandemic via newspapers and television (77.3%) (Table 1). The number of people living in the same residence ranged from 1-3 (46.5%), followed by 3-4 (42.4%). Most residences had 5-6 rooms (50.6%).
| Variables | n (%) |
|---|---|
| Age group (years) | |
| 18-39 | 35 (20.3) |
| 40-59 | 63 (36.6) |
| 60-87 | 74 (43.0) |
| Gender | |
| Female | 127 (73.8) |
| Male | 45 (26.2) |
| Race | |
| White | 67 (39.0) |
| Black | 22 (12.8) |
| Pardo (Brown) | 83 (48.3) |
| City of residence | |
| Goiania | 89 (51.7) |
| Others (Goias) | 83 (48.3) |
| Origin | |
| Interior of the state | 47 (27.3) |
| Metropolitan region | 121 (70.3) |
| Rural area | 4 (2.3) |
| Family income (minimum wage) | |
| = 1 | 76 (44.2) |
| 1-3 | 88 (51.2) |
| 3-5 | 8 (4.7) |
| Schooling | |
| Did not study | 11 (6.4) |
| Elementary school | 93 (54.1) |
| High school | 54 (31.4) |
| Higher education | 14 (8.1) |
| Have you been doing other leisure activities? | |
| No | 21 (12.2) |
| Yes | 151 (87.8) |
| Vehicle for obtaining information/guidance? | |
| Newspapers and TV | 133 (77.3) |
| Social networks | 34 (19.8) |
| Other | 5 (2.9) |
| How many people live in the household? | |
| 1-2 | 80 (46.5) |
| 3-4 | 73 (42.4) |
| 5-8 | 19 (11.0) |
| How many rooms does the residence have? | |
| 1-4 | 59 (34.3) |
| 5-6 | 87 (50.6) |
| 7-10 | 26 (15.1) |
n=absolute frequency; %=relative frequency
Table 1: Characterization of the sociodemographic profile and lifestyle habits of patients (n=172).
The most prevalent pathologies were asthma and COPD, accounting for 40.1% and 25.6%, respectively, followed by pulmonary hypertension (16.9%), non-cystic fibrosis bronchiectasis (5.2%) and cystic fibrosis (4.7%)
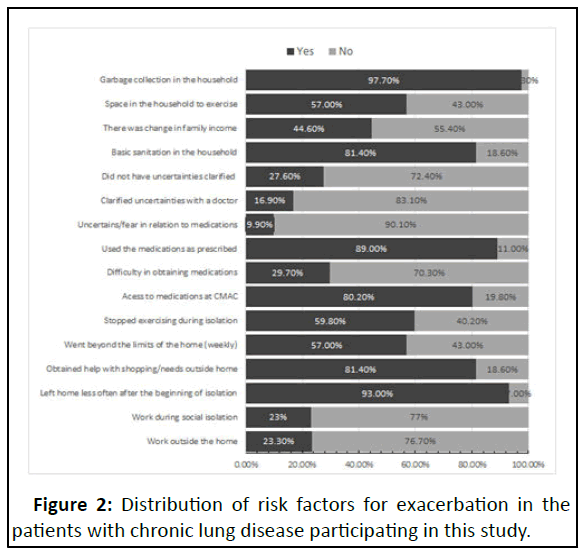
Most participants did not work outside the home during the social isolation period (77%) and after the social isolation period, there was a reduction of patients who worked outside the home (15%) as compared to before isolation (23%). Most people left homeless after the beginning of isolation (93%) and most said that other people did the shopping (81%) for the basic needs of the house. Regarding the treatment most had no difficulties in obtaining chronic medications and maintained their use as prescribed by the physician. In terms of physical activities, about half of the participants stopped doing exercise during social isolation (Figure 2).
We observed that 117 patients (68%) had no exacerbation during the study period. When we evaluated association between exacerbations and the sociodemographic profile, no association was found with gender, age, education, origin or family income. However, the prevalence of exacerbations was significantly higher (21.8%) among black patients than among those of other races (Table 2).
| Variables | Exacerbations n (%) | |||
|---|---|---|---|---|
| No | Yes | Total | p* | |
| n=117 (68.0) | n=55 (32.0) | n=172 | ||
| Age group | ||||
| 18 to 39 | 23 (19.7) | 12 (21.8) | 35 (20.3) | 0.28 |
| 40 to 59 | 39 (33.3) | 24 (43.6) | 63 (36.6) | |
| 60 to 87 | 55 (47.0) | 19 (34.5) | 74 (43.0) | |
| Gender | ||||
| Female | 89 (76.1) | 38 (69.1) | 127 (73.8) | 0.33 |
| Male | 28 (23.9) | 17 (30.9) | 45 (26.2) | |
| Race | ||||
| White | 47 (40.2) | 20 (36.4) | 67 (39.0) | 0.04 |
| Black | 10 (8.5) | 12 (21,8)‡ | 22 (12.8) | |
| Pardo (Brown) | 60 (51.3) | 23 (41.8) | 83 (48.3) | |
| Origin | ||||
| Interior of the state | 34 (29.1) | 13 (23.6) | 47 (27.3) | 0.7 |
| Metropolitan region | 80 (68.4) | 41 (74.5) | 121 (70.3) | |
| Rural area | 3 (2.6) | 1 (1.8) | 4 (2.3) | |
| Family income (minimum wage) | ||||
| = 1 | 52 (44.4) | 24 (43.6) | 76 (44.2) | 0.94 |
| 1 to 3 | 60 (51.3) | 28 (50.9) | 88 (51.2) | |
| 3 to 5 | 5 (4.3) | 3 (5.5) | 8 (4.7) | |
| Schooling | ||||
| Did not study | 7 (6.0) | 4 (7.3) | 11 (6.4) | 0.98 |
| Elementary School | 63 (53.8) | 30 (54.5) | 93 (54.1) | |
| High School | 37 (31.6) | 17 (30.9) | 54 (31.4) | |
| Higher education | 10 (8.5) | 4 (7.3) | 14 (8.1) | |
| Have you been doing other leisure activities | ||||
| No | 16 (13.7) | 5 (9.1) | 21 (12.2) | 0.39 |
| Yes | 101 (86.3) | 50 (90.9) | 151 (87.8) | |
| Vehicle for information/guidance | ||||
| Newspapers and TV | 92 (78.6) | 41 (74.5) | 133 (77.3) | 0.6 |
| Social networks | 21 (17.9) | 13 (23.6) | 34 (19.8) | |
| Other | 4 (3.4) | 1 (1.8) | 5 (2.9) | |
| How many persons in the household | ||||
| 1 to 2 | 56 (47.9) | 24 (43.6) | 80 (46.5) | 0.64 |
| 3 to 4 | 47 (40.2) | 26 (47.3) | 73 (42.4) | |
| 5 to 10 | 14 (12.0) | 5 (9.1) | 19 (11.0) | |
| How many rooms in the household | ||||
| 1 to 2 | 1 (0.9) | 1 (1.8) | 2 (1.2) | 0.81 |
| 3 to 4 | 38 (32.5) | 19 (34.5) | 57 (33.1) | |
| 5 to 10 | 78 (66.7) | 35 (63.6) | 113 (65.7) | |
Note: *: Chi-square; ‡: Post-hoc; n: Absolute frequency; %: Relative frequency
Table 2: Characterization and association of the presence of exacerbations with the sociodemographic profile and lifestyle habits of the participants in this study.
Regarding risk factors, there was a significantly higher frequency of exacerbations in those patients who sought physician advice to clarify uncertainties: 27.3% of patients who.
presented exacerbations clarified uncertainties with a physician. There was no difference in relation to physical activity, access to medications or isolation conditions (Table 3).
| Variables | Exacerbations | |||
|---|---|---|---|---|
| No | Yes | Total | p* |
|
| n=117 (68.0) | n=55 (32.0) | n=172 | ||
| Works outside the home | ||||
| No | 91 (77.8) | 41 (74.5) | 132 (76.7) | 0.64 |
| Yes | 26 (22.2) | 14 (25.5) | 40 (23.3) | |
| Worked during social isolation | ||||
| No | 53 (73.6) | 34 (82.9) | 87 (77.0) | 0.25 |
| Yes | 19 (26.4) | 7 (17.1) | 26 (23.0) | |
| Leaving home less after the beginning of isolation | ||||
| No | 6 (5.1) | 6 (10.9) | 12 (7.0) | 0.16 |
| Yes | 111 (94.9) | 49 (89.1) | 160 (93.0) | |
| Help for shopping/out-of-home needs | ||||
| No | 24 (20.5) | 8 (14.5) | 32 (18.6) | 0.34 |
| Yes | 93 (79.5) | 47 (85.5) | 140 (81.4) | |
| Goes out of the household (week) | ||||
| No | 48 (41.0) | 26 (47.3) | 74 (43.0) | 0.44 |
| Yes | 69 (59.0) | 29 (52.7) | 98 (57.0) | |
| Stopped exercising in isolation | ||||
| No | 27 (36.5) | 16 (48.5) | 43 (40.2) | 0.25 |
| Yes | 47 (63.5) | 17 (51.5) | 64 (59.8) | |
| Access to medication at CMAC | ||||
| No | 24 (20.5) | 10 (18.2) | 34 (19.8) | 0.72 |
| Yes | 93 (79.5) | 45 (81.8) | 138 (80.2) | |
| Difficulty in obtaining medications | ||||
| No | 86 (73.5) | 35 (63.6) | 121 (70.3) | 0.19 |
| Yes | 31 (26.5) | 20 (36.4) | 51 (29.7) | |
| Uses medications as prescribed | ||||
| No | 10 (8.5) | 9 (16.4) | 19 (11.0) | 0.12 |
| Yes | 107 (91.5) | 46 (83.6) | 153 (89.0) | |
| Doubt/fear regarding medications | ||||
| No | 106 (90.6) | 49 (89.1) | 155 (90.1) | 0.75 |
| Yes | 11 (9.4) | 6 (10.9) | 17 (9.9) | |
| Clarified doubts with a doctor | ||||
| No | 103 (88.0) | 40 (72.7) | 143 (83.1) | 0.01 |
| Yes | 14 (12.0) | 15 (27.3) | 29 (16.9) | |
| Any questions not answered | ||||
| No | 9 (64.3) | 12 (80.0) | 21 (72.4) | 0.34 |
| Yes | 5 (35.7) | 3 (20.0) | 8 (27.6) | |
Note: *: Chi-square; n: Absolute frequency; %: Relative frequency; CMAC: High-Cost Medication Center
Table 3: Characterization and association of the presence of exacerbations with risk factors for exacerbations and/or contamination of the participants in this study.
When we evaluated the patients' perception of their health status, we found a higher prevalence of exacerbations among patients who considered themselves unwell. There was a significant association between absence of exacerbations with the lowest grade of dyspnea (0-1) and the presence of exacerbations with the highest grades (2-3 and 4-5: 61.8% and 18.2%, respectively). The prevalence of exacerbations was identified in those patients who presented the highest amount of expectoration (grade 4-5: 14.5%) (Table 4).
|
Exacerbations |
|||
|---|---|---|---|---|
No |
Yes |
Total |
p* |
|
n=117 (68.0) |
n=55 (32.0) |
n=172 |
||
Consider themselves well |
||||
No |
5 (4.3) |
17 (30.9) |
22 (12.8) |
<0,01 |
Yes |
112 (95.7) |
38 (69.1) |
150 (87.2) |
|
Dyspnea |
||||
0-1 |
61 (52,1)‡ |
11 (20.0) |
72 (41.9) |
<0,01 |
2-3 |
43 (36.8) |
34 (61.8)‡ |
77 (44.8) |
|
4-5 |
13 (11.1) |
10 (18.2)‡ |
23 (13.4) |
|
Cough |
||||
0-1 |
74 (63.2) |
28 (50.9) |
102 (59.3) |
0.3 |
2-3 |
34 (29.1) |
21 (38.2) |
55 (32.0) |
|
4-5 |
9 (7.7) |
6 (10.9) |
15 (8.7) |
|
Quantity of sputum |
||||
0-1 |
90 (76.9) |
40 (72.7) |
130 (75.6) |
0.02 |
2-3 |
23 (19.7) |
7 (12.7) |
30 (17.4) |
|
4-5 |
4 (3.4) |
(14.5)‡ |
12 (7.0) |
|
Note: *: Chi-square; ‡: Posthoc; n: Absolute frequency; %: Relative frequency
Table 4: Characterization and association of the presence of exacerbations with health perception, dyspnea, cough and amount of sputum.
Initially, we observed that most of the interviewees did not have exacerbations during the period evaluated (68%). When we evaluated only patients with asthma and COPD, which are the group with the highest prevalence in the study, we noted that approximately 70% had no exacerbation. When we evaluated the association of diagnosis with exacerbation, we found no significant association.
Discussion
This study was conducted to evaluate the association between social isolation during the COVID-19 pandemic and the frequency of exacerbation in patients with chronic lung disease. Given the difficulty in achieving face to face contact with the patients, remote access was used for evaluation. Telemedicine had already been expanding for some years and was accelerated by the pandemic due to the urgent requirements of the situation [19]. A total of 172 patients were included in this study, constituting 38% of the patients scheduled at the XXX hospital pulmonology outpatient clinics during this period.
In our study, 97% of participants reported leaving home less frequently than before the pandemic. Many stopped working outside the home and some had shopping assistance for basic needs. A review performed at the Federal University of Bahia (UFBA) in April 2020 observed a major reduction in social mobilization, with a reduction of 70% in going to parks, by 71% in trade and recreation activities and by 64% in transport circulation, while about 34% of individuals stopped working outside the home. This is consistent with the findings in the present study, where most of the population avoided leaving home during the pandemic period.
There was a predominance of older individuals, women, lowincome and low education participants. A study conducted in Pelotas in patients with chronic no communicable diseases also showed a predominance of low income and low education participants [20]. These data are consistent with our study and may explain the difficulty in achieving telephone access and in participants’ ability to understand the questions asked during the interview in our study.
The most prevalent chronic lung diseases in our participants were asthma (40.1%), followed by COPD (25.6%) and pulmonary hypertension (16.9%). COPD and asthma are common respiratory diseases with a heterogeneous distribution and have the highest prevalence of lung diseases in the world [21].
Despite the pandemic, patients had no difficulty in obtaining the medications and maintaining their use as prescribed by the attending physician. The high cost inhaled medications that most patients use are provided by the Juarez Barbosa state center for high-cost medications (CEMAC). At the beginning of the pandemic, on March 23, 2020, CEMAC authorized automatic renewals for a period of 6 months, without the need for repeating examinations or presciptions [22]. This was one of the factors that made it possible for patients to continue accessing and using their medications regularly and continuously.
According to Dhruve et al., there was better adherence to Inhaled Cortico Steroids (ICS) in patients with asthma during the pandemic than in the years prior to the pandemic, particularly in older patients and in those at greater risk [23]. Poor adherence to inhaled medications, including ICS, was evaluated by a retrospective cohort study in 2006, showing adherence in less than 25% of participants in the period prior to the pandemic. In the present study, 89% of patients reported using medications as prescribed by their physician, which is a high adherence compared to previous data.
However, most patients and their physicians are likely to be familiar with the decline in asthma control that follows the emergence of respiratory viruses, such as SARS-CoV2 and hence, there is likely to be a degree of apprehension on both sides driving the observed increase to the good adherence to medication. Older patients and those aged over 65 years, in particular, have consistently demonstrated better ICS adherence than younger patients. These data are consistent with our study.
Old age was one of the first COVID-19 risk factors to emerge. These patients are also more likely to have other comorbidities, which further increases their risk for COVID-19. It is possible that older patients were therefore additionally encouraged to take their ICS regularly, as opposed to younger patients, who were considered to be at lower risk of the disease. In the current study, patients reported using the medications as prescribed by the physician in 89% of cases, which was a high adherence rate as compared to pre-pandemic data, particularly among older patients, indicating data consistent with the previous studies.
Most patients did not present exacerbation (68%) during the study period, which corroborates the data in the literature, where low exacerbation was observed after the beginning of social isolation measures in chronic lung disease patients [24]. In a multicenter study conducted in 2016 on asthma and COPD, 48.7% of the participants with COPD had exacerbation. In 2019, a longitudinal study of patients with severe asthma showed that 40% were likely to have an exacerbation.
In our study, 31% of the asthma patients and 25% of the COPD patients had exacerbations within the 3 months prior to the survey. This data can be explained by the lower risk of viral infections (SARS-CoV-2 and other viruses), by avoiding going out, using masks, avoiding crowds and implementing hand hygiene. In addition, another factor that may explain this result was the high adherence to continuous use medications, as prescribed by the physician, which is one of the main factors in controlling chronic lung diseases.
Regarding physical activity, previous studies have shown a reduction of exacerbation in patients with chronic lung disease who engaged in physical activity and cardiopulmonary rehabilitation. Seymour et al., randomized 60 patients with COPD and compared patients undergoing pulmonary rehabilitation with those under usual care. The found a reduced frequency of exacerbations in rehabilitation patients, in addition to increased exercise capacity and quality of life in these cases. Although physical exercise is fundamental for the reduction and prevention of exacerbations in chronic lung diseases, there was a reduction in the number of patients who continued exercising during social isolation in this study. There was no significant association of this variable with exacerbations. This is probably because there were other protective factors, such as better adherence to medication and less exposure to pathogens.
When we evaluated the association of exacerbation with the sociodemographic profile and lifestyle habits, we observed a significant association of exacerbations with black patients, but no association with the other variables. A study conducted in patients with asthma in California during the pandemic, from April to June 2020, observed a 78% reduction in hospitalization rate and 90% reduction in emergency room visits as compared with 2017 and 2019. However, this reduction was not observed in black patients. These data agree with our study. This can be explained by the lower socioeconomic and education levels among this population and the reduced access to healthcare and medication.
When assessing exacerbation association with the patient's perception of their health status, a significant association of exacerbations was verified among patients who considered themselves unwell. There was a significant association between the absence of exacerbations and the lowest grade of dyspnea (0-1) and between occurrence of exacerbations with the highest grades of dyspnea (2-3 and 4-5; 61.8% and 18.2%, respectively). The prevalence of exacerbations was identified in those patients who presented the highest amount of expectoration (grade 4-5; 14.5%).
These data showed that the patients with exacerbation actually presented more severe respiratory symptoms and that they had a good perception of the worsening of their symptoms, which justifies the fact that they sought doctors’ advice more often in order to clarify uncertainties and possibly treat the condition. This facilitates early treatment of exacerbations, avoiding hospitalizations or further complications of the underlying disease. It also suggests that patients with chronic lung disease have a good ability to recognize the need to seek medical care at the appropriate time, without unnecessary exposure to health services.
Conclusion
This study had some limitations. The difficulty of gaining telephone access, lack of ability of patients to understand the questions and remote rather than face to face access may have been some of the reasons for the small number of participants. The short evaluation period of about 3 months may have influenced the low number of exacerbations in the period, with most exacerbation studies ranging from 1 to 3 years of evaluation. In addition, the patients were not classified according to the severity of their underlying diseases or prior exacerbations, which may influence the outcome of the exacerbation.
The results of this study are of great social importance as it presents evidence of exacerbation reduction after the inception of virus containment measures during the pandemic. The use of masks and hand hygiene can prevent exacerbations and worsening of lung disease. These data encourage the continued use of these measures in some way, even after this period. Further studies are needed to obtain further evidence of these associations in chronic lung disease patients, to improve intervention planning and multidisciplinary management, with better follow-up and treatment in the post-pandemic period. Telemedicine was useful for patient evaluation and continues to be a particularly important tool at the present time, but it needs to be developed further and adapted to the reality of public hospitals.
References
- Singhal T (2020) Review on COVID19 disease so far. Indian J Pediatr 87:281-286
[Crossref] [Google Scholar] [PubMed]
- Perez-Campos Mayoral L, Hernandez-Huerta MT, Mayoral-Andrade G, Perez-Campos Mayoral E, Perez-Campos E (2020) World health organization declares global emergency: A review of the 2019 novel Coronavirus (COVID-19). Int J Surg 79:163-164
[Crossref] [Google Scholar] [PubMed]
- Bender BG, Pedan A, Varasteh LT (2006) Adherence and persistence with fluticasone propionate/salmeterol combination therapy. J Allergy Clin Immunol 118:899-904
[Crossref] [Google Scholar] [PubMed]
- Aquino EML, Silveira IH, Pescarini JM, Aquino R, de Souza-Filho JA (2020) Social distancing measures to control the COVID-19 pandemic: Potential impacts and challenges in Brazil. Cienc e Saude Coletiva 25:2423-2446
[Crossref] [Google Scholar] [PubMed]
- Benjamin D Granta, Chelsey A Smithb, Philip E Castlec, Michael E Scheurere, RR-K (2017) The Lung Microbiome, immunity and the pathogenesis of chronic lung disease. Physiol Behav 176:139-148
[Crossref] [Google Scholar] [PubMed]
- Miravitlles M, Anzueto A, Legnani D, Forstmeier L, Fargel M (2007) Patient’s perception of exacerbations of COPD-the PERCEIVE study. Respir Med 101:453-460
[Crossref] [Google Scholar] [PubMed]
- Chiu NC, Chi H, Tai YL, Peng CC, Tseng CY, et al. (2020) Impact of wearing masks, hand hygiene and social distancing on influenza, enterovirus and all-cause pneumonia during the coronavirus pandemic: Retrospective national epidemiological surveillance study. J Med Internet Res 22:32750008
[Crossref] [Google Scholar] [PubMed]
- Macintyre CR, Ahmad A (2020) A rapid systematic review of the efficacy of face masks and respirators against coronaviruses and other respiratory transmissible viruses for the community, healthcare workers and sick patients. Int J Nurs Stud 108:103629.
[Crossref] [Google Scholar] [PubMed]
- Liu S, Zhi Y, Ying S (2020) COVID-19 and asthma: Reflection during the pandemic. Clin Rev Allergy Immunol 59:78-88
[Crossref] [Google Scholar] [PubMed]
- Handa A, Dhooria S, Sehgal IS, Agarwal R (2018) Impact of COVID-19 on (Non-COVID) chronic respiratory disease outcome survey in India (CCROS study). Lung India 35:41-46
[Crossref] [Google Scholar] [PubMed]
- Caruso C, Colantuono S, Urbani S, Heffler E, Canonica GW, et al. (2021) Real-life survey on severe asthma patients during COVID-19 lockdown in Italy. Expert Rev Respir Med 15:1057-1060
[Crossref] [Google Scholar] [PubMed]
- Lee HH, Lin SH (2020) Effects of COVID-19 Prevention measures on other common infections, Taiwan. Emerg Infect Dis 26:2509-2511
[Crossref] [Google Scholar] [PubMed]
- Sabetkish N, Rahmani A (2021) The overall impact of COVID-19 on healthcare during the pandemic: A multidisciplinary point of view. Heal Sci Reports 4:1-12
[Crossref] [Google Scholar] [PubMed]
- MacDonald PL, Gardner RC (2000) Type I error rate comparisons of post hoc procedures for I × J chi-square tables. Educ Psychol Meas 60:735-754
- Mateo M, Alvarez R, Cobo C, Pallas J, Lopez A, et al. (2019) Telemedicine: Contributions, difficulties and key factors for implementation in the prison setting. Rev Espanola Sanid Penit 21:95-105
[Google Scholar] [PubMed]
- Soriano JB, Abajobir AA, Abate KH, Abera SF, Agrawal A, et al. (2017) Global, regional and national deaths, prevalence, disability-adjusted life years and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990-2015: A systematic analysis for the global burden of disease study 2015. Lancet Respir Med 5:691-706
[Crossref] [Google Scholar] [PubMed]
- Dhruve H, Ancona G, Holmes S, Dhariwal J (2020) Prescribing patterns and treatment adherence in patients with asthma during the COVID-19 pandemic hetal. J Allergy Clin Immunol Pract 10:100-107
[Crossref] [Google Scholar] [PubMed]
- Peters MC, Mauger D, Ross KR, Phillips B, Gaston B, et al. (2020) Evidence for Exacerbation-Prone Asthma and Predictive Biomarkers of Exacerbation Frequency. Am J Respir Crit Care Med 202:973–982
[Crossref] [Google Scholar] [PubMed]
- Metersky ML (2021) Fewer bronchiectasis exacerbations during the “lockdown” for COVID-19. Can we convert knowledge into action?. Am J Respir Crit Care Med 204:759-760
[Crossref] [Google Scholar] [PubMed]
- Han MK, Quibrera PM, Carretta EE, Barr RG, Bleecker ER, et al. (2018) Frequency of exacerbations in COPD: An analysis of the SPIROMICS cohort MeiLan. Ann Am Thorac Soc 5:619-626
[Crossref] [Google Scholar] [PubMed]
- Alsallakh MA, Sivakumaran S, Kennedy S, Vasileiou E, Lyons RA, et al. (2021) Impact of COVID-19 lockdown on the incidence and mortality of acute exacerbations of chronic obstructive pulmonary disease: National interrupted time series analyses for Scotland and Wales. BMC Med 19:1-10
[Crossref] [Google Scholar] [PubMed]
- Dadras O, Alinaghi SAS, Karimi A, MohsseniPour M, Barzegary A, et al. (2021) Effects of COVID-19 prevention procedures on other common infections: A systematic review. Eur J Med Res 26:1-13
[Crossref] [Google Scholar] [PubMed]
- Seymour JM, Moore L, Jolley CJ, Ward K, Creasey J, et al. (2010) Outpatient pulmonary rehabilitation following acute exacerbations of COPD. Thorax 65:423-428
[Crossref] [Google Scholar] [PubMed]
- Guijon OL, Morphew T, Ehwerhemuepha L, Galant SP (2021) Evaluating the impact of coronavirus disease 2019 on asthma morbidity: A comprehensive analysis of potential influencing factors. Ann Allergy, Asthma Immunol 127:91-99
[Crossref] [Google Scholar] [PubMed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences