Assessment of Prescribing Indicators in the Public and Private Sectors: A Cross-sectional Study in Twenty Community Pharmacies in an Urban Setting, Thỉ̮̬̉s, Senegal
Bassoum O1,2*, Sougou NM1,2, Lèye MM1,2, Dia O3, Faye A1,2 Seck I1,2, Fall D3 and Tal-Dia A1,2
1Department of Public Health and Preventive Medicine, Faculty of Medicine, Pharmacy and Odontology, University Cheikh Anta Diop, 5005 Dakar-Fann, Senegal
2Institute of Health and Development, University Cheikh Anta Diop, 16390, Dakar-Fann, Senegal
3Laboratory of Therapeutic and Organic Chemistry, Faculty of Medicine, Pharmacy and Odontology, University Cheikh Anta Diop, 5005, Dakar-Fann, Senegal
- *Corresponding Author:
- Oumar Bassoum
Institute of Health and Development
University Cheikh Anta Diop
16390, Dakar- Fann, Senegal
Tel: +221-33-824-98-78
Fax: +221-33-825-36-48
E-mail: bassoum.oumar@gmail.com
Received Date: October 11, 2018; Accepted Date: November 02, 2018; Published Date: November 07, 2018
Citation: Bassoum O, Sougou NM, Lèye MM, Dia O, Faye A, et al. (2018) Assessment of Prescribing Indicators in the Public and Private Sectors: A Cross-sectional Study in Twenty Community Pharmacies in an Urban Setting, Thiès, Senegal. J Clin Med Ther. 3:16.
Abstract
Introduction: Inappropriate prescribing practices are a major problem worldwide, especially in developing countries. Senegal has national drug policy and various tools to promote the rational use of medicines. However, little is known about their performance. We aimed to assess prescribing indicators in the public and private sectors.
Method: We carried out a cross-sectional study in an urban setting, Thiès. Our research ran from December 1, 2017 to January 16, 2018. A double sample was constituted. One consisted of 20 community pharmacies randomly selected using Microsoft Excel 2010. The other included 600 prescriptions. In each pharmacy, the first 30 prescriptions received on the day of the survey were recorded. The collection tool was WHO form 1. The analysis was done using Microsoft Excel 2010.
Results: A total of 600 prescriptions were recorded. The average number of medicines per prescription was 2.52. The percentage of medicines prescribed by an international nonproprietary name was 7%. Percentage of medicines prescribed from Senegal’s national essential medicines list was 32%. The use of antibiotics and injection was 40% and 7%, respectively. The results were almost similar between the public and private sectors.
Conclusion: Our study has demonstrated irrational prescribing practices in the public and private sectors in an urban setting. Capacity building of health professionals on the rational use of drugs is needed. Further studies would be necessary to better understand the extent of the problem and its determinants.
Keywords
Essential medicines; Rational use; Prescribing indicators; Community pharmacy; Public sector; Private sector; Thiès; Senegal
Introduction
Medicines contribute to the improvement of health and well-being when they are rationally used [1]. According to the World Health Organization (WHO), the rational use of medicines assumes that "patients receive medications appropriate to their clinical needs, in doses that meet their own individual requirements, for an adequate period of time, and at the lowest cost to them and their community"[2]. Conversely, irrational use occurs when these conditions are not met [1]. It exists in different forms such as polypharmacy, excessive use of antimicrobials and injections and unnecessary prescription of brand name drugs [1,3].
The irrational use of medicines is a major problem worldwide [3], especially in resource-poor countries [4]. WHO estimates that more than half of drugs are used inappropriately [4].
In the WHO African Region, recent studies have shown irrational prescribing practices [5,6]. This situation worsened in both public and private sectors between the periods 1995-2005 and 2006- 2015 [5].
The irrational use of medicines can be harmful to the patient and to economic resources [7]. It also impairs people's confidence in the health system [1].
In this situation, responsible use of medicines has long been considered a necessity [1]. For example, WHO has created an essential medicines list [8]. Essential medicines are regarded as those medicines that satisfy the priority health care needs of the population [3].
Next, it developed five prescribing indicators to monitor drug use [9]. It is about:
- Average number of medicines per prescription
- Percentage of medicines prescribed by generic name or international nonproprietary name (INN)
- Percentage of prescriptions with at least one antibiotic
- Percentage of prescriptions with at least one injection
- Percentage of drugs prescribed from essential medicines list or form
Similarly, the new sustainable development agenda advocates appropriate prescribing and use of medicines to ensure universal health coverage [10,11].
Senegal has also taken initiatives by implementing a national drug policy (NDP) [12], a national essential medicines list (NEML) [13], a handbook of therapeutic equivalences [14] and a drug database [15].
However, few studies are conducted to evaluate drug use in Senegal [16-18]. Thus, it became necessary to have new data to inform decision-making. Our study falls within this framework. The choice of our study concerns prescribing practices and is justified by the fact that the prescriber is an important actor who mainly intervenes at two levels of the cycle of medicine use such as diagnosis and prescribing [3]. Our objective was to evaluate the prescribing indicators in the city of Thiès and to compare them with WHO standards [5].
Methods
Study setting
The study took place in the city of Thiès. This city, located 70 km from Dakar, is the capital of the department and the region of the same name and is made up of three borough districts [19].
Its population was estimated at 354,386 inhabitants in 2017 [20].
According to the sanitary pyramid, the city of Thiès belongs to the health district of the same name. The number of health facilities is 45, of which 31 are in the public (27 health posts, 1 health center, 1 regional hospital and 2 military health facilities) and 14 in the private sector (8 health posts, 4 clinics, 2 denominational hospitals) [19,21].
The number of community pharmacies is 46 at the time of the study. The city hosts a faculty of medicine for training physicians and a regional health-training center for paramedics such as nurses and midwives [19].
Type of study and period of study
We conducted a cross-sectional, prospective study. Data were collected from December 1, 2017 to January 16, 2018.
Study population
The study population consisted of prescriptions received in community pharmacies in Thiès on the day of the survey.
Sampling
Selection criteria: The prescriptions included were those of patients treated on an outpatient basis. Parapharmaceutical products or vaccines were excluded from the study.
Sample size: Sampling was done according to WHO recommendations [22]. The number of community pharmacies required is twenty. In each of these pharmacies, we included 30 prescriptions. Thus, the size of the sample required was 600 prescriptions.
Sampling procedure: The list of community pharmacies in the city of Thiès served as a sampling frame for the random selection of the 20 community pharmacies. For this purpose, we used the Microsoft Excel 2010 to generate random numbers which were sorted in ascending order. The first 20 community pharmacies were included.
We included the first 30 prescriptions received at each community pharmacy on the day of the survey and meeting the inclusion criteria.
Data collection
Data collection tool: The survey tool was the WHO form 1 which was adapted to our study [22]. It was previously tested in one community pharmacy in Thiès. One form was provided for each community pharmacy. It consisted of eight columns. The first corresponded to prescription numbers ranging from one to thirty. The second column was used to record the name of each prescribed drug. The third was used to determine whether or not a drug is prescribed with an INN. It was coded 1 if the drug was prescribed by INN or 0 otherwise. The fourth and fifth columns identified prescriptions containing at least one antibiotic and at least one injection, respectively. The code 1 was assigned in case of presence of at least one antibiotic and at least one injection and 0 otherwise, respectively.
The sixth column allowed us to check whether or not the medicine was prescribed from the Senegal’s NEML. The presence was coded 1 and the absence 0.
Finally, columns 7 and 8 were related to the qualification of the prescriber (physician, dentist, nurse, midwife, dental assistant) and the origin of each prescription (public sector, private sector), respectively.
Data collection method: A prescriptions review was carried out. The Data were collected from the first 30 prescriptions presented in each community pharmacy. Every day was dedicated to a community pharmacy. The investigation began at 8 am until the required number of prescriptions was reached.
The data collector was a sixth-year pharmacy student at the Cheikh Anta Diop University in Dakar and assistant in a pharmacy in Thiès. He was trained on the data collection method and sensitized on the objectives of the study. The training materials were the data collecting form, WHO documents [9,22], the Senegal’s NEML [13], the handbook of therapeutic equivalences [14] and the drug database [15].
The investigator's tasks consisted of completing columns 1, 2, 4, 5, 7 and 8 while the supervisor completed columns 3 and 6.
Ethics
This study was conducted as of a Pharm. D thesis. It was an observational study and did not identify patients. The study did not involve any physical risk for patients and had no impact on the environment.
However, the informed consent of each patient was collected and the data were collected confidentially.
Statistics
The data were entered and analyzed using Microsoft Excel 2010.
The statistical analysis was descriptive. Quantitative variables were expressed as mean ± standard deviation, while qualitative variables were in percent.
The calculation of the five prescribing indicators was performed as follow [9]:
i) Average number of drugs per prescription=total number of different drugs prescribed divided by the number of prescriptions reviewed. Combination drugs are counted as one.
ii) Percentage of medicines prescribed by INN=number of medicines prescribed by INN divided by the total number of medicines prescribed and multiplied by 100.
iii) Percentage of medicines prescribed from Senegal’s NEML=number of medicines prescribed from Senegal’s NEML divided by the total number of drugs prescribed and multiplied by 100.
iv) Percentage of prescriptions with at least one antibiotic=number of prescriptions with at least one antibiotic divided by the number of prescriptions surveyed and multiplied by 100.
v) Percentage of prescriptions with at least one injection=number of prescriptions with at least one injection divided by the number of prescriptions surveyed and multiplied by 100.
Results
Prescription identification
A total of 600 prescriptions were included in our study. The number of prescriptions from public and private sectors was 417 (70%) and 169 (28%), respectively. However, the origin of 14 prescriptions (2%) was unknown (Table 1).
| Prescription identification | n | % |
|---|---|---|
| Sector Public sector |
417 | 70 |
| Private sector | ||
| Private for profit | 93 | 16 |
| Faith-based health care facilities | 76 | 13 |
| Unknown | 14 | 2 |
| Prescriber qualification | ||
| Physician | 237 | 40 |
| Dentist | 23 | 4 |
| Dental assistant | 12 | 2 |
| Nurse | 180 | 30 |
| Midwife | 81 | 14 |
| Unknown | 67 | 11 |
Table 1: Distribution of prescriptions according to the sector and the prescriber qualification, Thiès, Senegal, December 2017-January 2018 (N=600).
Prescribing indicators
The total number of medicines prescribed was 1513, of which 1063 (70.26%) and 414 (27.36%) were from public and private sectors, respectively. Half of the prescriptions contained at least three drugs. One prescription included 7 drugs (Table 2).
| Number of medicines | Global (N=600) | Public (N=417) | Private (N=169) | |||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| 1 | 112 | 19 | 81 | 19 | 30 | 18 |
| 2 | 191 | 32 | 124 | 30 | 62 | 37 |
| 3 | 198 | 33 | 139 | 33 | 52 | 31 |
| 4 | 77 | 13 | 54 | 13 | 22 | 13 |
| 5 | 16 | 3 | 14 | 3 | 2 | 1 |
| 6 | 5 | 1 | 4 | 1 | 1 | 1 |
| 7 | 1 | 0 | 1 | 0 | 0 | 0 |
Table 2: Prescription distribution by number of prescribed medicines, Thiès, Senegal, December 2017-January 2018 (N=600).
Average number of medicines per prescription
The average number of medicines per prescription was 2.52 ± 1.08 (Table 3). In the public sector, the average number of medicines per prescription was 2.55 while in the private sector it was 2.45 (Table 3).
| Prescribing indicators | Global | Public | Private | WHO standards |
|---|---|---|---|---|
| Average number of drugs per prescription ± sd | 2.53 ± 1.08 | 2.55 ± 1.08 | 2.45 ± 1.08 | <2 |
| Percentage of medicines prescribed by INN | 7% | 7.8% | 7% | 100% |
| Percentage of medicines prescribed from the Senegal’s NEML | 32% | 31% | 34.3% | 100% |
| Percentage of prescriptions with at least one antibiotic | 40% | 42% | 34% | <30% |
| Percentage of prescriptions with at least one injection | 7% | 7% | 7% | <20% |
Table 3: Prescribing indicators, Thiès, Senegal, December 2017-January 2018 (N=600).
Percentage of medicines prescribed by INN
The percentage of medicines prescribed by INN was estimated at 7%. It was almost identical in the public (7.8%) and private (7%) sectors (Table 3).
Percentage of medicines prescribed from the Senegal’s NEML
Only 32% of medicines were prescribed from the Senegal’s NEML.
Most prescriptions were written by physicians (40%) followed by nurses (30%). The prescriber qualification was not specified in 11% of cases (Table 1).
This percentage was 31% in the public sector versus 34.3% in the private sector (Table 3).
Percentage of prescriptions with at least one antibiotic
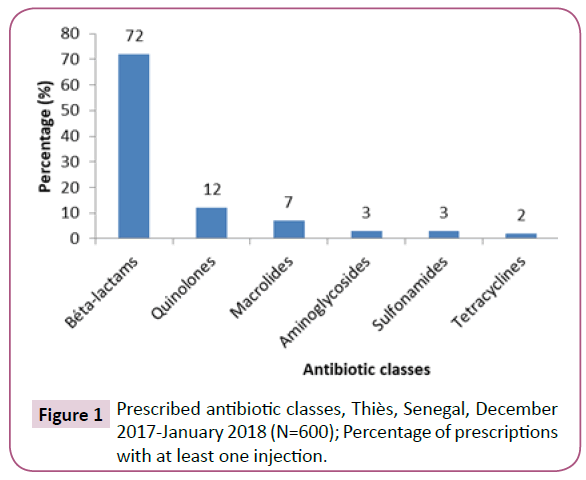
At least one antibiotic was prescribed in 40% of prescriptions including 42% in the public sector and 34% in the private sector (Table 3). The three most prescribed classes of antibiotics were beta-lactams (72%), quinolones (12% and macrolides (7%) (Figure 1).
The results of our study showed that 7% of prescriptions contained at least one injection. The same proportion was found in both the public and private sectors (Table 3).
Discussion
Since 2006, Senegal has a NDP document [12]. The main objectives of this NDP are, among others:
(i) To promote rational use of medicines by health professionals and consumers;
(ii) To promote research in the use of medicines;
(iii) To promote generic essential medicines to health workers and the general public
The NDP relies on various tools to rationalize the use of drugs. These are the NEML, handbook of therapeutic equivalences and Drug Database.
Senegal has a NEML since 1990. The last update dates from 2015. It is elaborated according to the levels of the health pyramid. It must be available in all health facilities in the public sector [13].
The handbook of therapeutic equivalences is developed in 2016 by the Senegal’s Pharmacy and Drug Department. It is the list of substitutable medicines in Senegal. The medicines listed therein are referred to by their brand name and INN. They are presented under their dosage, their pharmaceutical form, their route of administration and, secondarily, their conditioning [14].
The drug database is set up in 2017. It allows knowing the types of drugs marketed in Senegal, their indications and their price. It is available online on the website of the Senegal’s Pharmacy and Drug Department [15].
The purpose of this NDP and these tools is to promote availability and accessibility of essential medicines [12].
WHO recommends evaluating the performance of NDPs using core prescribing indicators [9]. Previous studies in Senegal showed shortcomings about availability of essential medicines and prescribing practices [16-18]. Our study, conducted in an urban setting, aimed to evaluate five key indicators of rational drug use both in public and private sectors. It has yielded important results and their implications in public health. These were compared with those found in previous studies. On the other hand, we compare them with the WHO optimal values, as well as with the results highlighted in other countries. These comparisons allow us not only to evaluate Senegal's performance in terms of rational use of medicines but also to guide decision-making for health system strengthening.
Average number of medicines per prescription
Our study showed that almost half (49.5%) of prescriptions contained at least three drugs. This has resulted in an average number of medicines per prescription equal to 2.52. In the public and the private sectors, this number was 2.55 and 2.45, respectively. These values do not comply with the WHO standard (<2). They have not changed much over time. In 1993-94, the average number of medicines per prescription was 3 in the region of Dakar and 2.3 in the rest of the country [17]. In 2003, it was estimated at 2.4 [18].
Slightly lower or comparable results were found in Ethiopia (2.34) [6], Egypt (2.5) [23] and Guyana (2.5) [24]. Higher results were found in Botswana (2.8) [25], Kenya (3) [26] and Nigeria (5.8) [27].
Our study revealed a tendency to prescribe several drugs (polypharmacy). Several causes are reported in the literature. It could be the lack of knowledge of health professionals [6], the aging of the population and the double burden of communicable and non-communicable diseases [5]. Polypharmacy- related problems are the occurrence of side effects and drug-drug interactions, which in turn can lead to treatment interruption or prescribing cascade [28]. The latter is described as an event that begins when an adverse drug reaction to a prescribed drug is interpreted as a new medical problem involving the prescription of a second drug, and so on [29].
In addition, polypharmacy is expensive in that it accounts for a large share of health expenditure [30]. In developing countries, health insurance schemes are weak [31]. Between 70% and 90% of drugs are paid by households at a cost representing 9.5% of their total expenditure [1,32]. Thus, the introduction of clinical guidelines would be essential in order to rationalize the number of drugs prescribed.
Percentage of medicines prescribed by INN
In our study, only 7% of drugs were prescribed by INN while the WHO standard is 100%. In 2003, this proportion was 60% [18].
This result is well below those found in the WHO African Region (68%) [5] and Botswana (78.6%) [25]. This situation could be explained by the influence of the medical representatives on the one hand [33,24] and the low level of knowledge among prescribers on the concept of generic medicine on the other hand [26]. At the same time, in the public sector, stocks out of drugs are recurrent in Senegal [34]. Thus, prescribers fall back on brand name drugs that are usually only available in community pharmacies.
INN prescribing has many advantages. It reduces the risk of confusion during dispensing [35] and facilitates communication between health professionals [36]. It also improves people's access to cheaper medicines [35].
Our study showed that the low use of INN prescribing remains a major challenge that it is urgent to meet. For this purpose, three strategies, among others, are necessary. First, prescribers should be made more aware of INNs by updating and disseminating documents such as the NEML, the handbook of therapeutic equivalences and the drug database. Second, independent drug information should be made available to limit the influence of medical representatives. Finally, the third strategy will be to promote the local production of generic and essential medicines.
Percentage of medicines prescribed from the Senegal’s NEML
According to our survey, the percentage of medicines prescribed from the Senegal’s NEML is low (32%). Paradoxically, it was slightly higher in the private sector (34.3%) than in the public sector (31%). In 2003, this indicator was estimated at 83.2% [18].
These results revealed a significant departure from the WHO standard (100%). This was also evident in India where only 37.3% [37] of the drugs belonged to an essential medicines list or form. However, in the WHO African Region, the use of the essential medicines list is higher (88%) [5]. In Nigeria, it is very close to the WHO standard (95.5%) [38]. In the Gambia, this value was 100% [39].
Our study highlighted a low adherence of prescribers to Senegal's NEML. In some countries, poor dissemination of essential medicines list and the influence of medical representatives have been demonstrated as factors that may explain this situation [5]. Further studies should be conducted to assess the availability of the latest version of the NEML among prescribers.
The use of a limited number of essential drugs allows rationalizing prescribing practices and costs of drugs [40]. Thus, the promotion of the concept of an essential medicines list would be necessary, especially in resource-limited countries [3].
Percentage of prescriptions with at least one antibiotic
In our study, 40% of prescriptions contained at least one antibiotic. This proportion was higher in the public sector (42%) than in the private sector (34%). The use of antibiotics has not generally evolved in Senegal since it was estimated at 39% and 46% in 1990 [16] and 2003 [18], respectively.
The results of our study exceeded the threshold set by WHO (<30%) and were comparable to those found in Botswana (42.7%) [25], Cameroon (36.71%) [41] and Pakistan (39.6%) [42]. On the other hand, they were lower than those highlighted in Vietnam (69%) and China (52.6%) [43].
In West Africa, the absence of a bacterial resistance monitoring system and a presumptive diagnosis established by prescribers who are often poorly trained are at the origin of inappropriate antibiotic prescribing [44]. For example, antibiotics are used for the treatment of respiratory infections, which are generally of viral origin [45]. In our study, those which were most prescribed belong to beta-lactams, quinolones and macrolides classes. Antimicrobial resistance, especially antibiotic resistance, is strongly associated with the irrational use of antibiotics and causes nearly 700,000 deaths per year [46].
Faced with this situation, it seems urgent to prevent the unnecessary consumption of antibiotics and reduce the burden of infectious diseases through effective policies [47]. These include the improvement of hygiene and sanitary conditions, vaccination, and access to high-performance diagnostic tools [47].
Percentage of prescriptions with at least one injection
This indicator was estimated at 7% in both the public and private sectors. The situation improved compared to that (25%) found in 2003 [18]. It complies with the threshold set by WHO (<20%). In India and Ghana, studies have also shown optimal use of injection with respective proportions of 7.2% [48] and 6.4% [49]. However, other studies have found higher results in sub-Saharan Africa (25%) [5], China (40.75%) [43] and Pakistan (27.1%) [50]. Excessive use of injection is recognized as a form of irrational use of drugs [1]. It exposes patients to infectious diseases transmitted by the blood and represents an additional workload for health professional [3,36]. In addition, injectable products are generally more expensive than oral forms [50].
The low rate of prescriptions with at least one injection demonstrated by our study represents an opportunity not only to reduce the incidence of blood-borne diseases but also to improve prescribing practices. In addition, population sensitization is essential because there is evidence in the literature that patients ask health workers to prescribe injection forms because of a misconception that the latter are more effective than oral forms [50]. At the regulatory level, one of the solutions would be to limit the prescription of injectable antibiotics in primary health care facilities [3].
Limits
The results of our study are not generalizable because of their very limited geographical and temporal character. On the one hand, the study only took place in an urban setting. On the other hand, we did it over a short period without taking into account seasonal variations. However, they represent new data on drug use in Senegal and will help in making-decision.
Conclusion
Our study has highlighted irrational prescribing practices both in the public and private sectors. These include polypharmacy, excessive use of antibiotics and prescribers’ low level of adherence to the concept of essential drugs. In contrast, the use of injections complies with the WHO optimal value.
The results of our study indicate the need for implementing interventions to promote rational use of medicines among prescribers. These include training prescribers, implementing clinical guidelines, updating and disseminating tools such as the Senegal’s NLEM, the handbook of therapeutic equivalences and the drugs database. Furthermore, it would be necessary to sensitize populations and to regulate pharmaceutical sector. Extensive studies in other regions of Senegal over a long period would be needed to better understand the extent of the problem and its determinants.
Conflict of Interest
The authors do not declare any conflict of interest.
Funding
This research received no external funding
Acknowledgement
We are very grateful to the community pharmacists who agreed to welcome us to their pharmacies. We also extend our warmest thanks to the patients/care-takers for giving us their prescription in order to register the drugs that are prescribed.
References
- Wirtz VJ, Hogerzeil HV, Gray AL, Bigdeli M, De Joncheere CP, et al. (2017) Essential medicines for universal health coverage. Lancet 389: 403-476.
- https://apps.who.int/medicinedocs/documents/s17054e/s17054e.pdf
- Ofori-Asenso R, Agyeman AA (2016) Irrational use of medicines-a summary of key concepts. Pharm 4: 35.
- Holloway KA, Ivanovska V, Wagner AK, Vialle‐Valentin C, Ross‐Degnan D (2013) Have we improved use of medicines in developing and transitional countries and do we know how to? Two decades of evidence. Trop Med Int Health 18: 656-664.
- Ofori-Asenso R, Brhlikova P, Pollock AM (2016) Prescribing indicators at primary health care centers within the WHO African region: a systematic analysis (1995-2015). BMC Pub Health 16: 724.
- Sisay M, Mengistu G, Molla B, Amare F, Gabriel T (2017) Evaluation of rational drug use based on World Health Organization core drug use indicators in selected public hospitals of eastern Ethiopia: A cross sectional study. BMC Health Services Res 17: 161.
- Farooqui R, Hoor T, Karim N, Muneer M (2018) Potential drug-drug interactions among patients’ prescriptions collected from medicine out-patient setting. Pak J Med Sci 34: 144.
- Woods H, Oronsaye E, Bali A, Rajakulasingam Y, Lee T, et al. (2018) Development of a provisional essential medicines list for children in Canada: Consensus process. CMAJ open 6: E146-E150.
- https://apps.who.int/medicinedocs/pdf/s2289e/s2289e.pdf
- https://apps.who.int/medicinedocs/documents/s23274en/s23274en.pdf
- https://apps.who.int/medicinedocs/documents/s23276fr/s23276fr.pdf
- https://apps.who.int/medicinedocs/documents/s18820fr/s18820fr.pdf
- https://www.mspp.gouv.ht/site/downloads/Liste%20Nationale%20des%20Medicaments%20Essentiels.pdf
- https://www.dirpharm.net/images/sampledata/pdf/GUIDE_SERECO_07_Mars_2016_Emma.pdf
- https://www.dirpharm.com
- https://apps.who.int/medicinedocs/fr/d/Jh2964f
- https://apps.who.int/medicinedocs/pdf/s2234f/s2234f.pdf
- https://apps.who.int/medicinedocs/documents/s16430f/s16430f.pdf
- https://www.ansd.sn/ressources/ses/SES-Thies-2013.pdf
- https://www.ansd.sn/ressources/publications/indicateurs/Projections-demographiques-2013-2025+.htm
- https://www.sante.gouv.sn/Les-r%C3%A9gions-m%C3%A9dicales/les-r%C3%A9gions-m%C3%A9dicales
- https://apps.who.int/medicinedocs/pdf/whozip15f/whozip15f.pdf
- Akl OA, El Mahalli AA, Elkahky AA, Salem AM (2014) WHO/INRUD drug use indicators at primary healthcare centers in Alexandria, Egypt. J Taibah Univ Med Sci 9: 54-64.
- Sharma S, Bowman C, Alladin-Karan B, Singh N (2016) Antibiotic prescribing patterns in the pediatric emergency department at Georgetown Public Hospital Corporation: a retrospective chart review. BMC Infectious Dis 16: 170.
- Mashalla Y, Setlhare V, Massele A, Sepako E, Tiroyakgosi C, et al. (2017) Assessment of prescribing practices at the primary healthcare facilities in Botswana with an emphasis on antibiotics: Findings and implications. Int J Clin Practice 71: e13042.
- Ambetsa MO, Oluka MN, Okalebo FA, Mulwa NC, Fadare J, et al. (2017) One-day out-patient prescribing patterns at a national referral hospital in Kenya. African J Pharmacol Ther 6: 96-101.
- Adisa R, Fakeye TO, Aindero VO (2015) Evaluation of prescription pattern and patients’ opinion on healthcare practices in selected primary healthcare facilities in Ibadan, South-Western Nigeria. African Health Sci 15: 1318-1329.
- Ahmadi F, Zarei E (2017) Prescribing patterns of rural family physicians: A study in Kermanshah Province, Iran. BMC Public Health 17: 908.
- Mallet L (2016) La cascade médicamenteuse: Comment la prévenir, la détecter et résoudre les problèmes qu ’elle engendre. Pharmactuel 49.
- Helali A (2006) Usage rationnel. Le bon usage des médicaments. Med Trop 66: 619-622.
- Gateaux V, Heitz JM (2008) L'accès aux médicaments: un défi pour l'industrie pharmaceutique. Humanisme et entreprise 13-28.
- Saouadogo H, Amoussou KM, Ouédraogo L (2012) Étude des mécanismes pérennes de financement des médicaments essentiels à Loumbila, Burkina Faso. Santé Publique 24: 365-377.
- Hassali MA, Wong ZY, Alrasheedy AA, Saleem F, Yahaya AHM, et al. (2014) Perspectives of physicians practicing in low and middle income countries towards generic medicines: a narrative review. Health Policy 117: 297-310.
- https://www.ouestaf.com/marche-du-medicament-au-senegal-autopsie-dun-secteur-en-crise-2/
- Ojo MA, Igwilo CI, Emedoh T (2014) Prescribing patterns and perceptions of health care professionals about rational drug use in a specialist hospital clinic. J Public Health Afr 5: 242.
- Cole CP, James PB, Kargbo AT (2015) An evaluation of the prescribing patterns for under-five patients at a Tertiary Paediatric Hospital in Sierra Leone. J Basic Clin Pharm 6: 109-114.
- Gopalakrishnan S, Ganeshkumar P, Katta A (2013) Assessment of prescribing practices among urban and rural general practitioners in Tamil Nadu. Indian J Pharmacol 45: 252.
- Umar LW, Isah A, Shuaibu Musa BU (2018) Prescribing pattern and antibiotic use for hospitalized children in a Northern Nigerian Teaching Hospital. Annals African Med 17: 26-32.
- Holloway KA, Henry D (2014) WHO essential medicines policies and use in developing and transitional countries: an analysis of reported policy implementation and medicines use surveys. PLoS Med 11: e1001724.
- Summoro TS, Gidebo KD, Kanche ZZ, Woticha EW (2015) Evaluation of trends of drug-prescribing patterns based on WHO prescribing indicators at outpatient departments of four hospitals in southern Ethiopia. Drug Design Dev Ther 9: 4551-4557.
- Anong DN, Akoachere JFK (2018) Prescribing patterns and associated factors of antibiotic prescription in primary health care facilities of Kumbo East and Kumbo West Health Districts, North West Cameroon. PloS one 13: e0193353.
- Atif M, Azeem M, Sarwar MR, Malik I, Ahmad W, et al. (2018) Evaluation of prescription errors and prescribing indicators in the private practices in Bahawalpur, Pakistan. J Chinese Med Association 81: 444-449.
- Mao W, Vu H, Xie Z, Chen W, Tang S (2015) Systematic review on irrational use of medicines in China and Vietnam. PloS one 10: e0117710.
- Ouedraogo AS, Pierre HJ, Banuls AL, Ouédraogo R, Godreuil S (2017) Émergence et diffusion de la résistance aux antibiotiques en Afrique de l’Ouest: facteurs favorisants et évaluation de la menace. Médecine et Santé Tropicales 27 : 147-154.
- Truter I (2015) Antimicrobial prescribing in South Africa using a large pharmacy database: A drug utilisation study Ilse Truter. Southern African J Infect Dis 30: 52-56.
- https://amr-review.org/sites/default/files/160525_Final%20paper_with%20cover.pdf
- Klein EY, Van Boeckel TP, Martinez EM, Pant S, Gandra S, et al. (2018) Global increase and geographic convergence in antibiotic consumption between 2000 and 2015. Proc Natl Acad Sci USA 115: E3463-E3470.
- Aravamuthan A, Arputhavanan M, Subramaniam K (2017) Assessment of current prescribing practices using World Health Organization core drug use and complementary indicators in selected rural community pharmacies in Southern India. J Pharm Pol Prac 10: 1.
- Prah J, Kizzie-Hayford J, Walker E, Ampofo-Asiama A (2017) Antibiotic prescription pattern in a Ghanaian primary health care facility.. Pan Afr Med J 28: 214.
- Atif M, Sarwar MR, Azeem M, Naz M, Amir S, et al. (2016) Assessment of core drug use indicators using WHO/INRUD methodology at primary healthcare centers in Bahawalpur, Pakistan. BMC Health Serv Res 16: 684.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences