Anti-Toxoplasma gondii IgG, IgM, and IgA among Type-2 Diabetic Patients in Benghazi Libya: A Comparison Study
1Department of Biology, Faculty of Education-Ghemines, University of Benghazi, Benghazi, Libya
2Department of Medical, Faculty of Medicine, University of Benghazi, Benghazi, Libya. The Endocrine Unit, Hawari General Hospital, Benghazi, Libya
- Corresponding Author:
- Eman Z Younis
Department of Biology, Faculty of Education-Ghemines
University of Benghazi, Benghazi
Libya
Tel: +218- 927783883
E-mail: Eman.younis@uob.edu.ly
Received date: August 10, 2018; Accepted date: October 26, 2018; Published date: October 30, 2018
Citation: Younis EZ, Elamami AH (2018) Anti-Toxoplasma gondii IgG, IgM, and IgA among Type-2 Diabetic Patients in Benghazi Libya: A Comparison Study J Immunol Microbiol. Vol.2 No.1.
Copyright: © 2018 Younis EZ, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
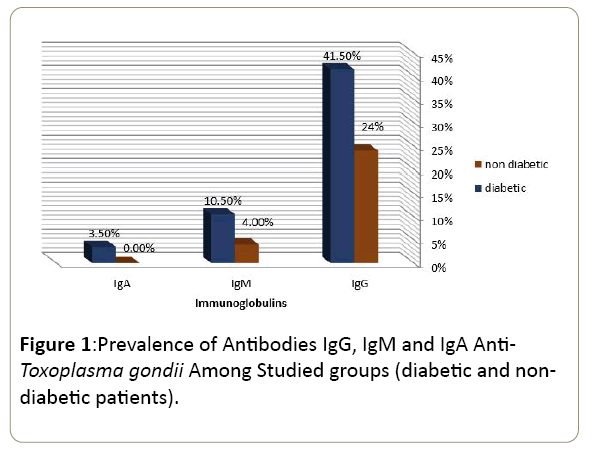
Toxoplasma gondii is an important opportunistic parasite in immune compromised hosts like Diabetes Mellitus (DM) patients. On other hand, diabetes is a systemic disease which affects the immune system, diabetes mellitus is an increasing problem in our country today and diabetics have been reported to be immunocompromised. Hence, detection and monitoring of anti-Toxoplasma antibodies are of a great interest in Diabetes Mellitus (DM) patients. Aim: To identify the prevalence of Toxoplasma gondii in Type 2 diabetic Patients using ELISA methods in Benghazi, Libya. Settings and Design: A case control study of Type 2 diabetic patients was conducted at Benghazi diabetic and endocrine centre between August to November 2016. Materials and Methods: Two hundred and fifty serum samples including 200 from diabetic Type 2 patients (125 Female and 75 Male) and fifty samples from healthy nondiabetics (32 Female and 18 Male) were used as a control group. A total of 250 blood samples were taken from individuals aged from 18 to<51 years. The Enzyme-Linked Immunosorbent Assay (ELISA), were used to detect Levels of IgG, IgM, and IgA antibodies against Toxoplasma gondii in the patients' sera. Cases and controls were matched for detection of Toxoplasma (Ab) with demographic parameter such as gender, age, abortion and the presence of wild animals especially cats. Statistical Analysis: Statistical analyses were performed using the Statistical Package for the Social Sciences version 17; SPSS Inc, Chicago, IL, USA). Results: The overall Prevalence of infection with Toxoplasma gondii among Type 2 diabetic patients [IgM=21 (10.5%), IgG=83 (41.5%) and IgA=7 (3.5%)] was higher than non-diabetics individual group [IgM=(4%), IgG=(24%) and IgA=(0%)].
Keywords
Toxoplasma gondii; ELISA; Diabetes; Benghazi; Libya
Introduction
Toxoplasmosis is a zoonotic infection caused by a ubiquitous intracellular protozoa parasite a Toxoplasma gondii, belonging to family Toxoplasmidae and Class Toxoplasmidae [1]. The protozoon infects different warm-blooded organisms, including human, birds, and rodents, as the intermediate hosts. Moreover, it infects domesticate and wild cats as the definite host [2,3].
Toxoplasma gondii generally, cause a self-limited, asymptomatic disease in immune competent patients, but is an important opportunistic parasite in immunocompromised people. Primary maternal infection during pregnancy can be transmitted to the foetus and result in serious sequelae (3) during the acute infection of toxoplasmosis, tachyzoites rapidly proliferate. In this stage, the parasite attacks the nucleated cell via active invasion. After proliferation, the tachyzoites destroy and kill the host cells and disseminate to the central nervous system, eyes, cardiac and skeletal muscles, and placenta via blood circulation. Finally, the immune system response causes transformation of the tachyzoites into bradyzoites, and the tissue cysts are developed. The tissue cysts remain alive and are able to sustain in the host body throughout the host lifespan. [4].
On the other hand, diabetes is the disease influences the cellular and humoral immunity predisposing the patient to many opportunistic parasites one of them is Toxoplasma gondii. It’s well known that Both diabetes and toxoplasmosis can cause congenital malformation of the foetus.
Consequently, the aim of our study focused on the serologic detection of Toxoplasma gondii infection in diabetic patients and compared to non-diabetic control.
Materials and Methods
Study design and Patients
A case control study was conducted in Benghazi city. The study has been done for 250 serum samples including 200 of them Type 2 diabetic patients (125 Female and 75 Male) recruited from government diabetes and endocrine centre (Syde Hussein) and 50 cases of healthy non-diabetics (32 Female and 18 Male) control group has been recruited randomly from the Alhaya laboratory during the period from August to November 2016. Cases and controls were matched with demographic parameters such as age, gender, abortion and the presence of wild animals especially cat’s and history of diabetic patients was recorded.
Methods
Antibody detection: Antibody detection using Elisa test to detect specific Toxoplasma antibodies and IgA.
Blood samples and preparation of sera: Blood samples were collected from the venepuncture of the patient into plain sterile tubes, left to clot at room temperature an hour, and centrifuged subsequently at 3000 RPM for at least 20 min at room temperature. the separated sera were stored at -20ºC or below until analysis of T. gondii by ELISA [5-7].
Determination of antibodies to T. gondii: All 250 serum samples were tested using Euroimmun enzyme-linked immunosorbent assay (ELISA) kits (PerkinElmer Company Euroimmun, Lübeck, Germany) for the presence of Toxoplasma IgG, IgM and IgA antibodies. Positive and negative controls were used with each series of anti T. gondii IgG/IgM/IgA test IgG and IgM and IgA indexes of<0.8 were regarded as the negative results, between 0.8 to 1.1 as the borderline, and ≥ 1.1 as the positive results, Positive IgG titers and negative IgM titers were considered a latent infection. Sera with concurrent positive IgG and IgM titers were further analysed by Elias test, results were obtained by reading the optical density at 450 nm using spectrophotometer and values were interpreted comparing with the cut-off value.
Data processing and analysis: Data was colleted and analyzed with Statistical Package for Social Sciences (SPSS) version 17 on Windows XP. Chi-square test was used to compare the differences in prevalence of Toxoplasma gondii Ab between the age groups, gender, abortion and the presence of wild animals. Data were considered statistically significant when the P-value was<0.05.
Results
In the present study out of 200 (38 positive and 162 negative) among Patients with Type 2 diabetic subjects who were tested (41.5%) were seropositive for Toxoplasma - IgG antibodies, 21/200 (10.5%) and 7/200 (3.5%) were seropositive for IgM and IgA antibodies, respectively, while in control group, 50 individuals 12 (24%) were positive for IgG and 2 (4%) IgM antibody. IgA antibody was negative for all samples of control group (0 %) (Table 1 & Figure 1).
| Diabetic | |||
|---|---|---|---|
| Immunoglobulins | Negative | Positive | Total |
| IgG | 117 (58.5%) | 83 (41.5%) | 200 |
| Ig M | 179 (89.5%) | 21 (10.5%) | 200 |
| IgA | 193 (96.55%) | 7 (3.5%) | 200 |
| Non diabetic | |||
| Immunoglobulins | Negative | Positive | Total |
| IgG | 38 (76.0%) | 12 (24%) | 50 |
| IgM | 48 (96.0%) | 2 (4.0%) | 50 |
| IgA | 50 (100%) | 0 (0.0%) | 50 |
Table 1: Prevalence of Antibodies IgG, IgM and IgA Anti- Toxoplasma gondii among studied group’s diabetic and nondiabetic patients.
The result shows no statistical difference in antibodies prevalence according to age either in diabetic or healthy nondiabetic control except for IgG level in diabetics where significantly higher in younger diabetic’s (IgG: X2=10.779a, P=0.013). Similarly, no statistical difference in antibodies prevalence according to sex in either group is shown in (Tables 2-4).
| Age group | No. of exam | IgM infected | IgG infected | IgA infected | Statistical difference of toxoplasma antibodies between age groups |
|---|---|---|---|---|---|
| (18-28) | 79 | 9 (11.4%) | 23 (29.1%) | 3 (3.8%) | IgG: X2 10.779a, P=0.013 |
| (29-39) | 84 | 10 (11.9%) | 39 (46.4%) | 4 (4.8%) | IgM: X2 1.812a, P=0.612 |
| (40-51) | 29 | 1 (3.4%) | 15 (51.7%) | 0 (0%) | |
| (>51) | 8 | 1 (12.5 %) | 6 (75.0%) | 0 (0%) | IgA: X2 1.759a, P=0.624 |
| Total | 200 | 21 (10.5%) | 83 (41.5%) | 7 (3.5%) |
Table 2 : Prevalence of Antibodies IgG, Ig M and IgA Anti-Toxoplasma gondii among diabetic patients according to age groups.
| Age group | No. of exam | IgM infected | IgG infected | Statistical difference of toxoplasma antibodies between age groups |
|---|---|---|---|---|
| (18-28) | 6 | 0 (0.0%) | 0 (0.0%) | IgG: X2 7.502a, P=0.058 |
| (29-39) | 11 | 0 (0.0%) | 3 (27%) | |
| (40-51) | 10 | 0 (0.0%) | 1 (10%) | IgM: X2 1.437a, P=0.697 |
| (52-62) | 23 | 2 (100%) | 8 (34.8%) | |
| Total | 50 | 2 | 12 |
Table 3: Prevalence of Antibodies IgG and IgM Anti-Toxoplasma gondii among non-diabetic patients according to age groups.
| Diabetic | |||||
|---|---|---|---|---|---|
| Sex | No. exam | IgM infected | IgG infected | IgA infected | Statistical difference of toxoplasma antibodies between age groups |
| M | 75 | 9 (12.0%) | 31 (41.3%) | 1 (1.3%) | Ig M: X2 0.287a, P=0.592 |
| F | 125 | 12 (9.6%) | 52 (41.6%) | 6 (4.8%) | IgG: X2 0.001a, P=0.970 |
| Total | 200 | 21 (10.5%) | 83 (41.5%) | 7 (3.5%) | IgA: X2 1.668a, P=0.197 |
| Non-Diabetic | |||||
| M | 18 | 1 (5.6%) | 6 (33.3%) | 0 | IgM: X2 3.391a, P=0.066 |
| F | 32 | 1 (3.1%) | 6 (18.8%) | 0 | IgG: X2 0.233a P=0.630 |
| Total | 50 | 2 | 12 | 0 | |
Table 4: Prevalence of Antibodies IgG, Ig M and IgA Anti- Toxoplasma gondii according gender among diabetic and nondiabetic participants.
Diabetic with domestic cat contact they have significantly higher antibodies (IgG, IgM, IgA) seropositivity compared to diabetic with no history of domestic cat contact. (IgM: X2=20.231a, df=1, P=0.00; IgG: X2=48.445a, df=1, P=0.000; IgA: X2=11.991a, df=1, P=0.001).While in non-diabetic only IgG was statistically different. (IgM: X2=.136a, df=1 P=.712; IgG: X=212.348a, df =1, p= 0.000) in (Tables 5 & 6).
| No. exam | IgG infected | IgM infected | IgA infected | |
|---|---|---|---|---|
| Contact with cat | 40 | 36 (90.0%) | 12 (30.0%) | 5 (12.5%) |
| Non-contact | 160 | 47 (29.4%) | 9 (5.6%) | 2 (1.3%) |
| Total | 200 | 83 | 21 | 7 |
Table 5: Prevalence of Antibodies IgG, IgM and IgA Anti- Toxoplasma gondii and contact with domestic cat among diabetic patients.
| No. exam | IgG infected | IgM infected | |
|---|---|---|---|
| Contact with cat | 15 | 6 (40.0%) | 1 (6.7%) |
| Non-contact | 35 | 6 (17.1%) | 1 (2.9%) |
| Total | 50 | 12 | 2 |
Table 6: Prevalence of Antibodies IgG and IgM Anti-Toxoplasma gondii and contact with domestic cat among non-diabetic participants.
The clinical inference of antibody status of all participant show (41.5%) have probably previous exposure to toxoplasmosis and (56%) seronegative and (10.5%) of recent infection, (3.5%) only IgA positivity of acute infection and others of probably of reactivated infection (Table 7).
| Inference | No. | % | Antibodies Status |
|---|---|---|---|
| Previous exposure | 83 | 41.5 | IgG (+) IgM (-) |
| Recently infection | 21 | 10.5 | IgM (+) IgG (-) |
| The IgA test is used by some laboratories as an additional marker of acute infection | 7 | 3.5 | IgA (+) |
| Reactivated? | 6 | 3 | IgA (+) IgG (+) IgM (+) |
| Reactivated or chronic T. gondii infection | 16 | 8 | IgG (+) IgM (+) |
| Seronegative | 112 | 56 | IgG (-) IgM (-) |
Table 7: The antibody status of the participant and their clinical inference.
Discussion
This is the first study aiming to determine anti toxoplasma antibodies in diabetic patients attending at government diabetes and endocrine centre in the city of Benghazi. In the present study out of 200 (38 positive and 162 negative) among Patients with type 2 diabetics who were tested, 41.5% were seropositive for Toxo- IgG antibodies,10.5% (21/200) and 3.5% (7/200) were seropositive for IgM and IgA antibodies, respectively, while in control group, 50 individuals 12 (24%) were positive for IgG and 2 (4%) IgM antibody. IgA antibody was negative for all samples of control group (0%) therefore; these findings suggest that diabetics are more susceptible to Toxoplasmosis than those without.
This result in agreement of which they found with Shirbazou et al. the prevalence of IgG antibodies against Toxoplasma gondii in diabetic patients and healthy controls were 60.43% and 38% respectively. Also in accordance with of Which demonstrate with Entsar J. Saheb that the seroprevalence of toxoplasmosis in diabetic patients was found to be comparatively higher than in non-diabetic patients [8,9].
The relation between diabetes and T. gondii infection is still poorly understood, in a study conducted by Arshad et al. the analysis revealed that Toxoplasma infection was more prevalent in diabetic patients than non-diabetic individuals. Results also showed that insulin level was higher in persons with chronic infection [10].
While in anon comparison study in Iran has shown that 70.3% among diabetic patients were seropositive for Toxoplasma antibodies [11]. Similarly, Gocke et al. study confirmed that 56% of diabetic patients were positive for anti-T. gondii IgG. [12].
The value of 24% seroprevalence of anti-T. gondii IgG in control group is lower to a study by Akinbami et al. in Nigeria 40.8 %.in non-diabetic pregnant women [13].
While the result of the current study is lower than 81.1% reported by Zemene et al. In the South western and Central Ethiopia respectively [14,15].
Similarly the results found in our study of anti-T.gondii IgM antibodies was 10.5% (21/200) was in higher compared to 5.3 % reported by Silva et al. [12,16].
IgA and IgM class antibodies are associated with recent infections (acute infection) while IgG class antibodies are associated with chronic infection. However, the IgA antibody test is not commonly used, and mostly used to detect the disease in cases of congenital infection. Thus, the IgA antibody test is an important marker for T. gondii infection in new born babies. In our study the anti-T. gondii IgA was low 3.5% compared to 69.4% reported by Fernando et al. in high risk pregnant female. However, in the current study the anti-T. gondii IgA was 0% in healthy control group which is similar to finding of Carmen et al among healthy individuals in Slovakia [17,18].
In contrast in a case control study in Durango City, Mexico they conclude that there is no serological evidence of an association between T. gondii infection and diabetes mellitus in the studied subjects [19].
A systematic review and Meta-analysis of case-control studies was published the researcher conclude that chronic toxoplasmosis as a possible risk factor for type 2 DM. However, based on random effects model no statistically significant association was observed between T. gondii and type 1 (DM).
The result shows no statistical difference in antibodies prevalence according to sex either in diabetic or non-diabetics, this in contrast to finding of Entsar J. Saheb [9]. The same finding with age except for IgG level in diabetics where significantly higher in younger diabetic’s (X2=10.779a, P=.013) which in agreement with Entsar J. Saheb.
Diabetic with history of cat contact they have significantly higher Toxoplasma antibodies (IgG, IgM, IgA) seropositivity compared to diabetic with no history of domestic cat contact, while in non-diabetic only IgG was statistically different.
A Meta-Analysis published at 2016, show that cat contact can increase the risk of infection by T. gondii in various populations, including the general population, immune-suppressed/pregnant individuals, those with special occupations, and cat(s) owners, but while significant, cat contact may not be the most important risk factor for infection by T. gondii in cat owners Wei HX et al. [20,21].
Conclusion
Anti-Toxoplasma gondii IgG, Ig M, and IgA levels among Type 2 diabetic Patients was higher than non-diabetic in Benghazi, Libya. Gender and age were not determining variable except for younger diabetic were the IgG was higher. History of domestic cat contact was risk variable for diabetics.
Acknowledgement
This research was supported and funded by Department of medical laboratory in Higher institute of medical. Benghazi, Libya. The authors are grateful to the members of the medical laboratory institute and the students which they aid in the collection of samples.
Disclosure
Funding
This work was funded by Department of medical laboratory in Higher institute of medical. Benghazi, Libya.
Conflict of interest
No conflict of interest.
References
- World Health Organization (1969) Toxoplasmosis: Report of a WHO meeting of investigators. World Health Organ Tech Rep Ser 431: 1-30.
- Dubey JP, Lindsay DS, Speer CA (1998) Structures of Toxoplasma gondii tachyzoites, bradyzoites, and sporozoites and biology and development of tissue cysts. Cli Micro Rev 11: 267-299.
- Montoya JG, Liesenfeld O (2004) Toxoplasmosis. Lancet 363: 1965-1976.
- Montoya JG, Liesenfeld O, Kinney S, Press C, Remington JS (2002) VIDAS test for avidity of Toxoplasma-specific immunoglobulin G for confirmatory testing of pregnant women. J Clin Microbiol 40: 2504-2508.
- CDC/NIH Interagency Working Group (1993) Biosafety in Microbiological and Biomedical Laboratories. 3rd Edition. U. S. Dept. of Health and Human Services, Public Health Service. 18-24.
- National Committee for Clinical Laboratory Standards (1990) Procedures for the Collection of Diagnostic Blood Specimens by Venipuncture Approved Standard. NCCLS Publication H18-A.
- Alford CA, Stagno Jr. S, Reynolds DW (1974) Congenital toxoplasmosis: Clinical, laboratory, and Therapeutic considerations, with special reference to subclinical disease. Bull NY Acad Med 50: 160-181.
- Shirbazou S, Delpisheh A, Mokhetari R, Tavakoli G (2013) Serologic Detection of Anti Toxoplasma gondii Infection in Diabetic Patients. Iran Red Crescent Med J 15: 701-703.
- Entsar JS (2017) Detection of toxoplasmosis infection in diabetic patients. DJM 12: 70-74.
- Arshad M, Cheema KJ, Malik HJ, Sajjad S (2017) The probable relation between Toxoplasma gondii and diabetes mellitus. Pakistan J of Sci Vol 69: 202-206.
- Goekce C, Yazar S, Bayram F, Gundogan K (2008) Toxoplasma gondii antibodies in Type 1 diabetes mellitus. Turkiye Klinikleri J 28: 619-622.
- Modrek MJ, Saravani R, Mousavi M, Alireza KS, Piri M (2015) Investigation of IgG and IgM antibodies against Toxoplasma gondii among diabetic patients. Int J Infect 2: e27595.
- Akinbami AA, Adewunmi AA, Rabiu KA, Wright KO, Dosunmu AO, et al. (2010). Seroprevalence of Toxoplasma gondii antibodies amongst pregnant women at the Lagos State University Teaching Hospital, Nigeria. Niger Postgrad Med J 17: 164-167.
- Zemene E, Yewhalaw D, Abera S, Belay T, Samuel A, et al. (2012). Seroprevalence of Toxoplasma gondii and associated risk factors among pregnant women in Jimma town, Southwestern Ethiopia. BMC Infect Dis 12: 337.
- Gebremedhin EZ, Abebe AH, Tessema TS, Tullu KD, Medhin G, et al. (2013). Seroepidemiology of Toxoplasma gondii infection in women of child-bearing age in Central Ethiopia BMC Infect Dis 13: 101.
- Silva MG, Vinaud MC, Castro AM (2015). Prevalence of toxoplasmosis in pregnant women and vertical transmission of Toxoplasma gondii in patients from basic units of health from Gurupi, Tocantins, Brazil, from 2012 to 2014. PlosOne 10: e0141700.
- Fernando HAM, Ferreira MN, Camargo NS, Santos GS, Spegiorin LCJ et al. (2016) Frequency of anti- Toxoplasma gondii IgA, IgM, and IgG antibodies in high-risk pregnancies, in Brazil , Rev. Soc. Bras. Med Trop.49: 512-514.
- Carmen S, Gabriela B, Renata H, ((2006) )Seroprevalence of Toxoplasma gondii antibodies in a healthy population from Slovakia. European Journal of Internal Medicine 17: 470-473.
- Murata FH, Ferreira MN, Camargo NS, Santos GS, Spegiorin LC, et al. (2016) Frequency of anti- Toxoplasma gondii IgA, IgM, and IgG antibodies in high-risk pregnancies, in Brazil. Rev. Soc. Bras Med Trop 49: 512-514.
- Majidiani H, Dalvand S, Daryani A, Galvan-Ramirez ML, Foroutan-Rad M (2016) Is chronic toxoplasmosis a risk factor for diabetes mellitus? A systematic review and meta-analysis of case-control studies. Braz J Infect Dis 20: 605-609.
- Wei HX, He C, Yang PL, Lindsay DS, Peng HJ (2016) Relationship between cat contact and infection by Toxoplasma gondii in humans: A meta-analysis. Comp Parasitol 83: 11-19.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences