ISSN : 2576-3938
Journal of Emergency and Internal Medicine
Anticipated Difficult Tracheostomy: Should CT Scan Be a Pre-Requisite
Kanwalpreet Sodhi*
Department of Critical Care, SPS Hospitals, Ludhiana, Punjab, India
- *Corresponding Author:
- Kanwalpreet Sodhi
Senior Consultant, Department of Critical Care
SPS Hospitals, Ludhiana, Punjab, India
Tel: 0161 661 7111
E-mail: drkanwal2006@yahoo.com
Received Date: October 24, 2017 Accepted Date: October 26, 2017 Published Date: October 28, 2017
Citation: Sodhi K (2017) Anticipated Difficult Tracheostomy: Should CT Scan Be a Pre-Requisite. J Emerg Intern Med Vol.1 No.2:14.
Abstract
Tracheotomy is a surgical procedure which consists of making an incision on the anterior aspect of the neck and opening a direct airway through an incision in the trachea. In our case, surgical tracheostomy was planned because of anticipated difficulty neck anatomy.
Literature suggests that although tracheotomy is a commonly performed procedure; however, with anatomical deformities, it can be associated with a high morbidity and mortality, partially due to accidental decannulation potential difficulties exist with both surgical tracheostomies performed on obese patients with short/thick necks and prolonged intubation.
This report shows that clinical examination and CXR imaging can be misguiding. CT scan is not routinely required for short, thick neck but if any problem is being faced during ventilation or for likely difficult tracheostomies, especially with some obvious unfavourable neck anatomy like anterior neck swellings, CT neck can be a useful guide.
We want to emphasize that we should have a low threshold for CT scan before tracheostomy to avoid unanticipated complications.
Keywords
Craniotomy; Tracheostomy tube; 3D spiral CT
Introduction
Tracheostomy is a frequently performed procedure in intensive care unit (ICU), aimed to maintain a patent airway in a patient. Sound knowledge of indications, operative techniques, risks, and complications is crucial as the procedure is associated with immediate life-threatening or subtle late potential complications [1].
Case Presentation
A 65-year-old diabetic, hypertensive female presented to our hospital with alleged history of fall from height and GCS of 5 (E1V1M3). CT head showed left subdural hemorrhage for which craniotomy was done. Patient was on ventilatory support and in view of need for prolonged ventilation, tracheostomy was planned.
Due to a thyroid swelling in front of neck, surgical tracheostomy was asked for. On surgical dissection under general anesthesia, it was a difficult tracheostomy - both thyroid lobes were enlarged and 7.00 mm cuff tracheostomy tube was inserted with difficulty. Bilateral air entry was equal. Patient was shifted back to ICU and put on volume control ventilation.
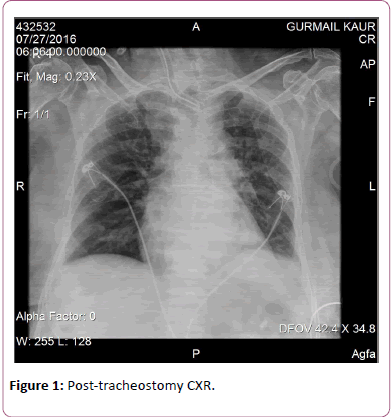
A leak was detected in inspiratory and expiratory tidal volumes, but chest expansion was adequate and bilateral air entry was present with SpO2 of 92% to 94% on FiO2 of 0.4. Post-procedure CXR did not reveal any complication (Figure 1). It was decided to insert a larger sized tracheostomy tube. Repositioning of tube was done by railroading a larger sized 7.5 mm, longer tracheostomy tube with adjustable flange (Portex) over the bougie.
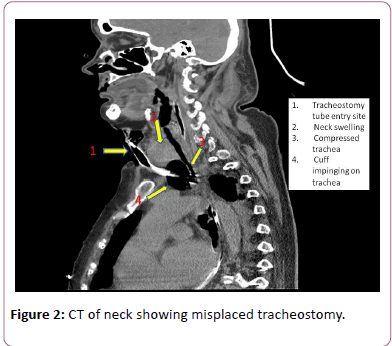
Patient could be ventilated but still significant leak was detected on the ventilator. CT neck was planned to look for exact tracheostomy tube positioning. CT neck showed the cuff of tube placed just outside the trachea, impinging upon the anterior tracheal wall and tip just inside the tracheal opening (Figure 2).
It was observed that the tracheostomy tube was following a tortuous course because of the thyroid swelling. After discussion with the surgeon, looking at the CT neck, tracheostomy repositioning was planned through the lower tracheal ring, which would be a straighter course for the tracheostomy. Patient was intubated after removing the original tracheostomy tube.
In the operating room, an 8.00 mm normal tracheostomy tube was positioned by percutaneous technique at the level of lower tracheal ring. No air leak was detected. Repeat CT imaging confirmed the appropriate tracheostomy position. Patient was weaned off the ventilator after two days and subsequently uneventfully discharged after eight days with tracheostomy in-situ.
Discussion
In our case, surgical tracheostomy was planned because of anticipated difficulty neck anatomy. But even with open exploration, great difficulty was encountered in placing the tracheostomy tube. Eventually a longer tube was put in, which also was supposedly not long enough for the anteroposterior length of neck. Also, the incision was likely at a higher level which led to a more tortuous course. This was proved by the CT scan that showed the cuff to be lying outside the trachea and a long subcutaneous course of the tube. Our patient continued to be ventilated, most likely from the tip of the tracheostomy tube just at the opening in the trachea and we could visualize a chest rise.
Literature also suggests that although tracheotomy is a commonly performed procedure; however, with anatomical deformities, it can be associated with a high morbidity and mortality, partially due to accidental decannulation. Walker, in a retrospective study on 293 patients showed that the measurement of the depth of pre-tracheal soft tissue DPST on CT does predict those patients in need of an extended-length tracheotomy tube [2]. Tsitouridis showed in a study on 13 patients that three-dimensional spiral CT reconstructions are a valuable adjunct of transverse images for the evaluation of trachea in cases of suspected tracheal tube-related complications [3.] Hwang and colleagues reported a case report on an obese woman with short neck where Sagittal CT scan showed that the trachea followed the course of the cervical and thoracic spine and not the direction of the skin contour, and that the curvature of the spine was quite pronounced [4]. As a result of which the extrathoracic trachea lied deep in the root of neck. The case was managed subsequently using an endotracheal tube exchanger. They also concluded that tracheostomies in obese individuals are usually fraught with difficulties because of the size discrepancy and curvature mismatch between a standard-size tracheostomy tube and the increased distance between the skin and trachea.
Conclusion
In conclusion, potential difficulties exist with both surgical tracheostomy performed on obese patients with short/thick necks and prolonged intubation. This report shows that clinical examination and CXR imaging can be misguiding. CT scan is not routinely required for short, thick neck but if any problem is being faced during ventilation or for likely difficult tracheostomies, especially with some obvious unfavourable neck anatomy like anterior neck swellings, CT neck can be a useful guide. We want to emphasize that we should have a low threshold for CT scan before tracheostomy to avoid unanticipated complications.
References
- Cipriano A, Mao ML, Hon HH, Vazquez D, Stawicki SP, et al. (2015) An overview of complications associated with open and percutaneous tracheostomy procedures. Int J Crit Illn Inj Sci 5: 179-188.
- Walker RN, Alexander IJ, Sartorius JA, Woomert CA (2012) Anthropometric measurements: Effect of CT depth of pretracheal soft tissue on tracheotomy tube selection. Am J Neuroradiol 33: 449-452.
- Tsitouridis I, Michaelides M, Dimarelos V, Arvaniti M (2009) Endotracheal and tracheostomy tube-related complications: Imaging with three-dimensional spiral computed tomography. Hippokratia 13: 97-100.
- Hwang SM, Jang JS, Yoo JI, Kwon HK, Lee SK, et al. (2011) Difficult tracheostomy tube placement in an obese patient with a short neck - A case report. Korean J Anesthesiol 60: 434-436.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences