An Unusual Case of Aggressive Angiomyolipoma Invading the Left Renal Vein
Vital Rangashamanna*, Maria Andrea Parra Corral, Ronald T Smith and Howayda Al Mrad
Department of Radiology, Texas Tech University Health Sciences Center, Lubbock, TX, United States
- *Corresponding Author:
- Vital Rangashamanna
Department of Radiology,
Texas Tech University Health Sciences Center,
Lubbock,
TX,
United States,
Tel: 9154721729;
E-mail: drvitalr@gmail.com
Received date: December 23, 2022, Manuscript No. IPCRCR-22-15475; Editor assigned date: December 26, 2022, PreQC No. IPCRCR-22-15475 (PQ); Reviewed date: January 10, 2023, QC No. IPCRCR-22-15475; Revised date: March 14, 2023, Manuscript No. IPCRCR-22-15475 (R); Published date: March 22, 2023, DOI: 10.36648/IPCRCR.7.1.001
Citation: Rangashamanna V, Corral MAP, Smith RT, Mrad HA (2023) An Unusual Case of Aggressive Angiomyolipoma Invading the Left Renal Vein. J Clin Radiol Case Rep Vol:7 No:1
Abstract
Renal angiomyolipomas are the most common benign renal neoplasms containing smooth muscle, adipose tissue and blood vessels. In the vast majority of cases those lesions are an incidental finding and are asymptomatic. In small percent of cases the lesions may be symptomatic presenting with backpain, hematuria and spontaneous hemorrhage being the most common complication. On rare occasions angiomyolipomas can be found to be angioinvasive extending in to the renal vein, inferior vena cava or right atrium. In this case report we describe a case of a 34 years old woman presenting with angiomyolipoma of the left kidney with invasion of the renal vein.
Keywords
Angiomyolipomas; Sclerosis; Neurofibromatosis; Luminal obstruction; Nephrectomy; Phacomatoses
Introduction
Renal Angiomyolipomas (AML) are benign lesions that are composed of smooth muscle, adipose tissue and abnormal blood vessels [1]. The majority of AMLs cases present as unilateral solitary lesions with no identified genetic association; on the contrary patients with multiple lesions in both kidneys are usually associated with phacomatoses such as tuberous sclerosis complex.
In more than 80% AMLs are detected incidentally on crosssectional imaging obtained for other medical conditions. The appearance is typically characteristic with majority of lesions appearing as solid lesions with demonstrable macroscopic fat. In 5% of lesions without macroscopic fat (fat poor AML), the diagnosis may be challenging as these lesions can be indistinguishable from renal cell carcinomas [2].
Symptomatic cases of AML are usually complicated by spontaneous retroperitoneal hemorrhage and present with back pain with or without associated hematuria. The severity of hemorrhage is variable from minimal to extremely severe bleeding with hemorrhagic shock (Wunderlich syndrome) [3]. Risk of AML associated hemorrhage is proportional to the size of the lesion with prophylactic embolization suggested for lesions exceeding 4 cm in diameter [4,5].
Angioinvasion of renal AML in to renal vein, Inferior venacava is a rare subset of aggressive AML’s with only about 90 cases reported worldwide [6]. Aggressive AML are more commonly been described to be affecting the right kidney [7]. In this case report we present a case of aggressive AML involving the left kidney and extending into the renal vein.
Case Presentation
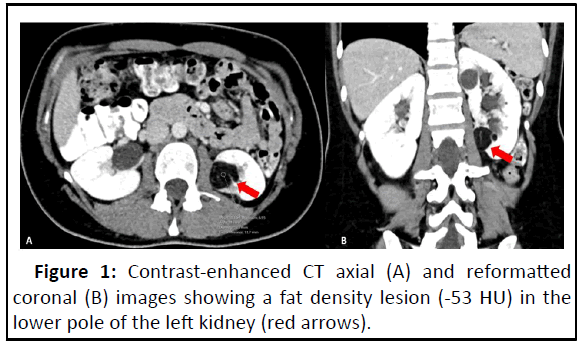
A 34 years old woman with no significant medical or surgical history was referred to outpatient radiology for evaluation of flank pain. A computer tomography of the abdomen and pelvis with intravenous contrast was performed. No prior imagings were available for comparison (Figure 1).
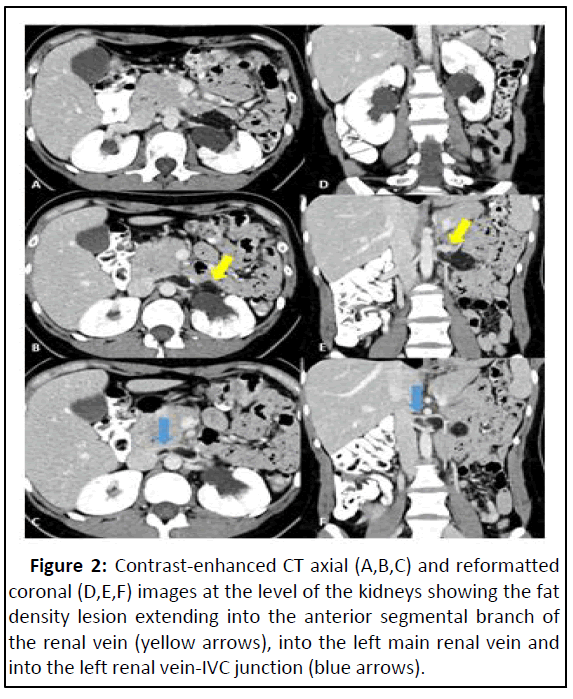
The computer tomography demonstrated a small isolated 3 cm fat density lesion in anterior cortex of the lower pole of the left kidney (measuring -53 Hounsfield units). The lesion was extending in to the left renal vein and propagating to the junction of renal vein and Inferior venacava causing partial luminal obstruction (Figure 2).
Figure 2: Contrast-enhanced CT axial (A,B,C) and reformatted coronal (D,E,F) images at the level of the kidneys showing the fat density lesion extending into the anterior segmental branch of the renal vein (yellow arrows), into the left main renal vein and into the left renal vein-IVC junction (blue arrows).
Results and Discussion
Renal AMLs are benign lesions containing smooth muscle, adipose tissue and blood vessels. These tumors have an estimated prevalence of 0.2%-0.6% with a female predilection, presenting commonly during their fourth to fifth decade of life. They can occur sporadically (80% of cases) or in association with phacomatoses, with vast majority in the setting of tuberous sclerosis complex, but also described in the setting of von Hippel-Lindau syndrome (vHL) and Neurofibromatosis type 1 (NF1). Sporadic type is the most common and found to be single lesions, in comparison when found in association with tuberous sclerosis complex it commonly affects both kidneys with multiple scattered lesions [8].
Renal AMLs have been classified into two subtypes: The classical subtype which is benign, and the epithelioid subtype which has been found to have a more aggressive behavior. Around three quarters of aggressive cases occur sporadically with one quarter associated to tuberous sclerosis complex. Aggressive variants have been more commonly seen in right kidney and are centrally located.
Renal AMLs are usually an incidental finding during sonographic or computer tomography evaluation obtained for other medical conditions. The majority of patients are asymptomatic, symptomatic patients usually have a larger lesion. Lesions can vary in size and grow slowly, AMLs are considered large if they measure ≥ 4 cm and can present with a palpable renal mass, abdominal pain, hypertension, renal failure or hemorrhagic shock (Wunderlich syndrome). As the likelihood of rupture significantly increases with size and complications are more commonly seen with tumors that measure more than 8 cm.
Epithelioid variant of AML has been associated with a more aggressive behavior, which has been described in very rare occasions. Aggressive behavior can be indicated as a lesion extending into the renal vein, inferior vena cava, right atrium and collecting system [9]. There was no association between the tumor aggressiveness and the size of the lesion in one of the case series published by Yiu, et al.
Due to their macroscopic fat content, AMLs can be found on ultrasound as hyperechoic renal masses. Computer tomography has a good sensitivity and specificity for accurately diagnosing AML, a classic AML will have around-15HU or less, demonstrating fat within a renal lesion is pathognomonic for AML. On rare occasions, around 4%-5% of AMLs can contain very little amount of fat which can present a diagnostic challenge as they can mimic renal cell carcinoma. Unenhanced CT scan study demonstrating increased density and MRI study demonstrating decreased T2 signal intensity of lipid pool AML compared to renal cell carcinoma can be of utility [10]. Nevertheless, percutaneous biopsy should be performed when differentiation of these tumors is not clear at CT or MRI.
Conclusion
Asymptomatic AMLs or small (<4 cm) are usually not treated and can be followed up annually with computer tomography or ultrasound. AML treatment is considered for lesions that are symptomatic, large (≥ 4 cm), with aggressive behavior (irrespective of size) or complicated AMLs (with hemorrhagic shock). Treatment for small or growing AMLs can include radiofrequency ablation or cryoablation. Treatment for tumors with a more aggressive behavior includes nephrectomy, either partial or radical. AMLs that invade the renal vein have a higher risk of thromboembolic complications including pulmonary embolism in which caval thrombectomy can be performed or inferior vena cava filter can be placed prior to nephrectomy.
References
- Yiu WC, Chu SM, Collins RJ, Tam PC, Chan FL, et al. (2002) Aggressive renal angiomyolipoma: Radiological and pathological correlation. J HK Coll Radiol 5:240-242
- Abou Heidar N, Degheili JA, Khauli RB, Abi Saad G (2020) A large bi-lobed classic renal AML with vena cava extension. Radiol Case Rep 15:353-361
[Crossref] [Google Scholar] [PubMed]
- Moratalla MB (2009) Wunderlich’s syndrome due to spontaneous rupture of large bilateral angiomyolipomas. Emerg Med J 26:72
[Crossref] [Google Scholar] [PubMed]
- Celik SU, Kocaay AF, Sevim Y, Cetinkaya OA, Atman ED, et al. (2015) Renal AML with caval extension and pulmonary fat embolism. Medicine 94:e1078
[Crossref] [Google Scholar] [PubMed]
- Shen G, Mao Q, Yang H, Wang C (2014) Aggressive renal AML with vena cava extension: A case report and literature review. Oncol Lett 8:1980-1982
[Crossref] [Google Scholar] [PubMed]
- Bakshi SS, Vishal K, Kalia V, Gill JS (2011) Aggressive renal AML extending into the renal vein and inferior vena cava–an uncommon entity. Br J Radiol 84:e166-e168
[Crossref] [Google Scholar] [PubMed]
- Kassimi M, Amriss O, Guerroum H, Habi J, Belhaj K, et al. (2021) Renal AML with renal vein extension. Radiol Case Rep 16:2325-2327
- Chenyang W, Xinyuan L, Linglong P, Xin G, Jing F (2018) An update on recent developments in rupture of renal angiomyolipoma. Medicine 97:e0497
[Crossref] [Google Scholar] [PubMed]
- Park BK (2017) Renal angiomyolipoma: Radiologic classification and imaging features according to the amount of fat. Am J Roentgenol 209:826–835
[Crossref] [Google Scholar] [PubMed]
- Kheir P, Abdessater M, El Khoury J, Akiel R, El Hachem C, et al. (2020) Renal angiomyolipoma with IVC thrombus: A case report. Int J Surg Case Rep 70:149-153
[Crossref] [Google Scholar] [PubMed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences