ISSN : 2321-2748
American Journal of Phytomedicine and Clinical Therapeutics
An Overview of the Literature in Aromatherapy: Is the Olfactory System a Suitable Gateway for Modification of the Breathing Patterns (Mental Imagery & Tidal Valium) in COVID-19?
1Department of Physiology and Pharmacist, Reproductive Health Research Centre, Tehran University of Medical Sciences, Tehran, Iran
2Department of Bio-material Engineering, Chemical and Environmental Engineering, Engineering Faculty, University Putra Malaysia, 43400 Serdang, Selangor, Malaysia
- *Corresponding Author:
- Farideh Zafari Zangeneh
Department of Physiology and Pharmacist
Reproductive Health Research Centre
Tehran University of Medical Sciences
Tehran, Iran
Tel: +982166581616
E-mail: Zangeneh14@gmail.com
Received Date: August 28, 2021; Accepted Date: September 25, 2021; Published Date: October 02, 2021
Citation: Zangeneh FZ, Shoushtari MS (2021) An Overview of the Literature in Aromatherapy: Is the Olfactory System a Suitable Gateway for Modification of the Breathing Patterns (Mental Imagery & Tidal Valium) in COVID-19? Am J Phytomed Clin Ther Vol.9 No.10:44
Abstract
Background: Shortness of breath is a medical term for dyspnoea, which is often referred to as "air hunger" on occasion. The distressing sensation of dyspnoea has the greatest potential for inducing psychological damage. Air hunger begins to activate brain pathways that are known to play a role in post-traumatic stress disorder (PTSD), anxiety, and depression.
Objective: Aromatherapy can associate with the olfactory images in the nerve modulation process, and then it can be an effective respiratory and psychiatric rehabilitation against air hunger in COVID-19.
Methodology: Until April 2021, a PUBMED study was performed. Aromatherapy, respiratory pattern, mental imagery, anxiety disorders, and COVID-19 were some of the concepts used in the search.
Results: Mental imagery is a common occurrence in most people's daily lives. In this study, we proposed aromatherapy as an adjunct therapy to relieve anxiety on patients in before and post hospitalized with the COVID-19 by using advances in neuroscience and recognition of mental images. A wide range of psychological disorders can be relieved with the help of aromatherapy at the beginning of the patient's stress, fear, and depression.
Conclusion: Aromatherapy can be used in conjunction with the olfactory imagery in the nerve stimulation phase to produce a synergistic therapeutic effect on the neuro-pharmacological response to COVID-19 anxiety. Mental imagery motivates and engages when planning enjoyable and rewarding activities. Aromatherapy is a relaxation technique that increases the tidal volume of the lungs, which decreases air hunger, the patient is relieved by the aroma of the brain image, which is pleasurable to him. As a result, aromatherapy combined with a pleasant mental image can help to improve breathing patterns in dyspnea. Therefore, aromatherapy can be a type of respiratory/psychiatry rehabilitation for recovery tidal valium in dyspnea before and post hospitalized of patients with COVID-19.
Keywords
Aromatherapy; COVID-19; Olfactory mental imaging; Breathing pattern; Psychological disorders
Introduction
Cognition is in several parts of the world, the COVID-19 outbreak hit hard and fast, posing a serious threat to public health. SARSCoV- 2, a new coronavirus with a proclivity for the lower respiratory tract, can cause acute respiratory syndrome and is a serious cause for hospitalization. The method of breathing is often referred to as pulmonary ventilation. This rhythm is inextricably linked to the odour sensory modality in mammals. The rhythm of life is the rhythm of breathing.
Nasal Functions: Respiration and Olfaction
Respiration
The nasal cavity is an airway for breathing that connects to the Central Nervous System (CNS) through rhythmic neural activity. SARS-CoV-2, the new coronavirus for the lower respiratory tract, can cause Acute Respiratory Distress Syndrome (ARDS) with the need to hospitalize patients. Pulmonary ventilation is usually defined as the process of breathing. Unfortunately, this process for air hunger is the most distressing form of dyspnoea [1]. Ventilation, by its mechanical nature, depends on the exchange of alveolar gases and the function of two important muscles, the diaphragm and the intercostal muscles. Lung-protective ventilation may be the most important therapeutic technique for ARDS caused by the virus. Lung-protective ventilation reduces pulmonary complications and improves outcomes in patients with ARDS that need continuous ventilator assistance in the ICU by using additional physiological tidal volumes and avoiding high inspiratory pressures [2]. The most distressing symptom for someone who holds his breath for a long time is air hunger, which is often stated by ventilation patients. A manually ventilated patient does not have the choice of ending a voluntary breathhold immediately. Mechanical Ventilation (MV) can damage the lungs and diaphragm, and excessive air restriction can cause stress and anxiety, as well as be used as a form of punishment, such as waterboarding [3]. In 24 hours after intubation, up to 53% of MV patients developed Ventilator-Induced Diaphragmatic Dysfunction (VIDD), according to several recent reports. VIDD is a major clinical problem that often results in poor clinical outcomes [4]. The feeling of being deprived of oxygen can be linked to Post- Traumatic Stress Disorder (PTSD), which is common among ICU survivors. Air hunger is triggered by an increase in the cerebral cortex's predicted medullary respiratory drive (outcome drive), which is alleviated by a tidal velum increase in the lungs, which is sensed by vagal pulmonary stretch receptors. Therefore, inflammation and collapse in the lung units stimulate the afferent nerves in lung induces extra drive, and contributes to the sensation of dyspnoea, "which was present in 21 of the 24 Seattle ICU patients on initial presentation [5]. Dyspnoea (sob) should not be relieved by the respiratory tract, particularly when the tidal volume is low, because air hunger is not caused by increased work of respiration.
Normal respiration is closely linked to other functions such as energy liberation, carbonaceous material combustion, oxygen consumption, and, most importantly, carbon dioxide production. Injury and ARDS are caused by a disruption in lung haemostasis. The Pathogenesis of ARDS with an uncontrolled inflammatory response in the lungs, characterized by activation of alveolar macrophages/neutrophils, and increased permeability of alveolar capillary membranes and pulmonary edema high concentrations of proteases and other proteins that can disrupt alveolar diffusion. The proliferation of intercellular junctions and the development of fibrin-containing hyaline membrane in alveolar ducts and airways cause extensive pneumocystis necrosis and swelling of endothelial cells. In the latter stages, neutrophils and other inflammatory cells infiltrate the alveolar capillaries and smaller pulmonary arteries, followed by fibrin us thrombi [6]. Since pneumonia is associated with a shift in the alveolar haemostatic equilibrium, disturbance of bronchi-alveolar homeostasis should be avoided. Is aromatherapy, as a scientificartistic procedure, capable of assisting in the maintenance of pulmonary homeostasis? Can aromatherapy help control respiratory homeostasis? In other words, can the mental image of the scent be effective in conditions such as respiratory muscle fatigue or decreased respiratory function?
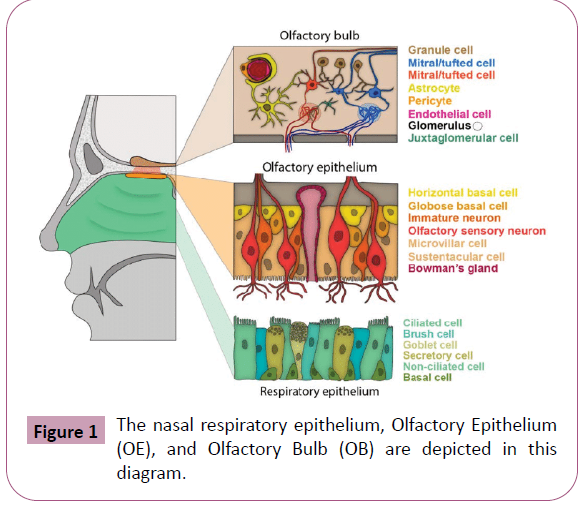
Olfaction
Olfaction is the oldest phylogenetic ally sensory modality, and its anatomical organization sets it apart from other sensory modalities [7]. Sensory transduction from the nose by olfactory afferent undergoes sophisticated processing in the olfactory bulb, particularly after Olfactory Epithelium (OE) sensory transduction. Even when there are no odours, the Olfactory Bulb (OB), as the first central processing stage of odours will rise and fall the triggering rates with each breath in a normal complex pattern [8]. Odour molecules are constantly present in our environment and can influence our feelings, values, and attitudes by stimulating our OB. Odour receptors (OR) are essential in the coalescence of axons of Olfactory Sensory Neurons (OSNs) from the Olfactory Epithelium (OE) to the Olfactory Bulb (OB). The axons of OSNs converge in only two to three molecularly specific glomeruli [9]. Each glomerulus is targeted by olfactory receptor neurons, which express a type of olfactory receptor protein. The olfactory glomeruli with a unique structure are at the forefront of the synaptic processing of olfactory information. According to the Cajal's catalogues, about 2,000 glomeruli cover surface of the OB. In the olfactory coding circuit, they are variously regarded as an organized functional unit. The size of the olfactory bulb varies greatly between vertebrate classes, and it is frequently used as a representation of olfactory abilities [10]. Anosmia is a temporary or permanent loss of this capacity that can be caused by allergies or a cold (brain tumours or head trauma). Anosmia may be one of the first symptoms of a coronavirus infection. While anosmia is not usually dangerous, it can have a significant impact on one's quality of life. When comparing pre-COVID imaging to post-COVID imaging, only one new case of COVID-19 after 2 months of anosmia with conclusive olfactory bulb atrophy has been identified [11]. However, Brann DH, et al. [12] found that certain COVID-19 patients had abnormal olfactory activity. They looked at bulk and single-cell RNA-Seq datasets to see which cell types in the (OE) and (OB) express COVID-19 infection-mediating cell entry molecules. They found that only the EP in mouse and human express two main genes involved in CoV-2 entry, ACE2 and TMPRSS2, neither OSNs nor OB neurons express these genes. They hypothesized that the anosmia disruptions caused by COVID-19 infection are caused by non-neuronal cell types such as axillary cells and Bowman gland cells, which are olfactory epithelial support cells (Figure 1). Primary multisensory and sensorymotor signals are combined and arranged at various levels of the neurological hierarchy to differentiate them neurologically in many dimensions, according to neuropsychological research. Using the sense of sight, hearing, taste, smell, touch and feeling, a mental image with sensory features can be developed. For example, what happens when you imagine or read the name of a lemon, which causes saliva to secrete? The mental image can be associated with pleasant and worried feelings. Employing mental imagery has a more potent influence on positive or negative emotions compared to verbal processing of the same information [13] and is practiced as more real than verbal processing [14]. Mental imagery permits us to pre-practice impending activities and thus to believe their potential to be pleasant and rewarding [15]. Renner F, et al. [16] in 2019 showed that mental imagery is an essential constituent of the prospective brain as an efficient network permitting us to predict and strategy for the future.16 Participants with mental imagery simulation presented a stronger enhancement of the all amounts assessing motivational aspects of the planned activities like motivation and anticipated pleasure/ reward) from pre to post activity planning. In these processes attention is the most important element in the creation of mental images. Mental imagery has been amplified according to the attention, so allowing for a greater positive or negative effect. Such images can have profound physiological effects for example about smelling sense. Djordjevic J, et al. [17] in 2005 showed that odour imagination is related to increased activation in some olfactory areas of the brain include the Primary Olfactory Cortex (POC) region [(piriform cortex, the Posterior Orbitofrontal Cortex (OFC)], and the rostral insula bilaterally. In addition, blood flow in two areas in the right orbitofrontal cortex was significantly correlated with behavioural measurements of odour images during scanning. The results revealed that the neural networks involved in detecting smell and images overlap to some degree. According to the findings of many studies, good odours are correlated with a greater sniffing response than unpleasant odours. Inhalation, whether smelling or perceiving a particular odour, may alter breathing patterns through imaging and olfactory perception. Klee Mann reported that breathing parameters such as respiratory minute volume, respiratory amplitude, and breathing rate on 56 healthy individuals. Their findings included volume and depth of respiration influenced by four distinct pleasant scents: rose flower, banana, lemon, and coffee. They found that olfactory perception and the baseline condition, as well as olfactory imagery and the baseline condition, resulted in a substantial increase in respiratory minute volume (p <0.001). Also in the respiratory amplitude there was a significant differences between imagery and baseline condition and between Odour and imagery condition, respiratory depth increases when (p <0.001) odour perception is significantly increased compared to baseline conditions. (p=0.002). They suggested that both olfactory perception and olfactory imagery affect the human respiratory profile with a common underlying mechanism [18]. According to a study by Rouby C, et al. [19] there is a strong connection between imaging ability and olfactory volume. As a result, people with strong mental imagery inhale more than those with poor mental imagery. While Kleemann AM, et al. [17] reported that olfactory imagery has no impact on the number of breaths and does not alter it, which is consistent with the findings of Djordjevic's research [18], but Masaoka Y, et al. [20] in 2012 reported that olfactory imagery has effect in the appearance of odour linked to autobiographical memories and control odour. Minute ventilation, tidal length, respiratory frequency, O2 intake, and end tidal CO2 concentration were among the respiratory factors assessed. Their findings revealed that retrieval of autobiographical memory is linked to increased tidal volume and decreased respiratory frequency as compared to the appearance of control odour. The most efficient way to fight shortness of breath (dyspnoea) is to increase the level of respiratory tidal volume.
Aromatherapy
History
René-Maurice Gattefossé, a French chemist, coined the term aromatherapy in the 1920s to describe the therapeutic effects of essential oils [21]. Terrenes make up the majority of essential oil constituents. Mono-terpenes and tetra-terpenes are classified according to the number of isoprene units (C5H8) in the molecule [22]. Plant essential oils are inhaled and applied topically to the skin. Drinking essential oils is the most efficient way to consume them since they enter the nose through two pathways: the mouth and the stomach. In the skin and digestive system, GABA Aminobutyric Acid (GABA) receptors and Transient Receptor Potential (TRP) channels appear to play a key role, but in the olfactory system, signals are largely transmitted to the olfactory bulb and the brain [23].
Odour nature and odour features
The amount of Odour received by the receptors is determined by the nature of the Odour, which includes concentration, adsorption rate (hydrophilic/hydrophobic), moisture, Odour evaporation rate, and airflow [24]. Physiological factors such as olfactory sense (the number of olfactory neurons involved in signal transduction), hormones and neuromodulators, and even an individual's lifestyle are all factors to consider [25]. All of these characteristics, as well as the Odour nature, must be managed or taken into account while utilizing aromatic compounds. It is the single olfactory receptors that determine the detection threshold (ORs). G-protein coupled receptors (GPCRs) are the biggest signalling protein superfamily in the genome, and they are found throughout the body. There is an expression of "sensory GPCRs" from the bitter taste receptors (TAS2R) family [26], and the olfactory receptors family in Human Airway Smooth Muscle (HASM) cells, deep in the lung [27].
Olfactory Receptors (ORs) Expression in the Non-Olfactory System
Since the early 1990s, olfactory receptors have been found to be expressed in non-olfactory tissues include: skin [28], heart [29], kidney [30] gastro-intestinal [31], testes [32] and sperm cells [33]. Olfactory receptor 2AT4 (OR2AT4) is another member of the olfactory receptors (ORs) family which was expressed in human skin and the outer basis sheath of hair follicles. OR2AT4 was stimulated by Sandal ore as synthetic sandalwood odourant. This essential oil can increase the healing process of epidermal wounds by repairing human skin through the signal cascade pathway of Mitogen-Activated Protein Kinase (MAPK) [34]. MAPK families plays a significant role in complex cellular programs include proliferation, differentiation, development, transformation, and apoptosis [28]. These findings imply that when essential oils are consumed or applied topically, ORs interact with them.
Interaction between Coronavirus and ORS
Anosmia is a well-described symptom of COVID-19. Numerous viruses of respiratory system are able to cause post-viral olfactory dysfunction as a sensor neural damage. Since the olfactory bulb is considered an immunological organ contributing to prevent the invasion of viruses, it could have a role in host defence. The local inflammatory products in COVID-19 by local damage cause olfactory loss simultaneously may interfere with the viral spread into the central nervous system (CNS). Therefore, ORs can be having a significant role as an alternative way of SARS-CoV-2 entry into cells locally, in CNS and systemically. Rate of these changes in olfactory bulb can be dependent to age/sex and comorbidity with the different exposure to infection. Torbay suggested that local TNF-α significantly increased in the olfactory epithelium in COVID-19, which its inflammation can lead to OR impairment, and damage to olfactory neurons [35]. Yao L, et al. [36] highlighted viral damage to OB and other areas of the brain through magnetic resonance imaging that was associated with olfactory function with OB volume in patients with COVID-19. The nasal epithelium and olfactory bulb are the first battlefields between coronavirus and the host. The consequence of this battle can be serious in the progress of the pathology of COVID-19. Respiratory rhythm as the vital rhythms of life is inextricably connected to olfaction.
Neurons in the OB are the first line of the central processing stage of Odour, their rhythmically rise and decline their firing rates with each breath, even in the lacks of odour. Therefore, respiration generates a continuous rhythmic neuronal input to the olfactory cortex (perform) [8]. For example, exposure (5 min) to the unpleasant Odour can induce a negative mood with mild anxiety, while exposure to the pleasant Odour can induce positive mood with calming [37]. The unique architecture of recognizing Odour, to form memory-based images (mental imagery), leads to the real perception of it. There is no capacity for olfactory imagery and respiratory rhythm generates a continuous rhythmic neuronal input to the perform, prefrontal cortex and the hippocampus for memory consolidation [38]. Thus, the pattern of respiratory rhythm is not only influenced by emotions but also by a two-way relationship between body and mind.
Olfactory Mental Imagery
Mental imaging has the potential to be a useful tool in the treatment of mood disorders and anxiety. Neuromodulator, particularly non-invasive brain stimulation for depression, could be a viable approach to psychiatric comorbid therapy. One of the most important strategies for patients to develop self-regulation is mental imagery. Patients can use the neuron feedback system to access this unique technology, which automatically adjusts activation in specific parts of the brain and networks. Is mental imaging and its unique relationship to emotional states, able to benefit the nervous patient?
Using developments in neuroscience and identification of mental images, as well as expanding evidence of its usefulness, notably in emotional and anxiety disorders, this study offers aromatherapy as an additional therapy to alleviate anxiety in patients hospitalized with the COVID-19 virus. Aromatherapy can help with a wide range of psychiatric disorders, especially if used early in stress, fear, or distress. What is the relationship between aromatherapy and psychological disorders?
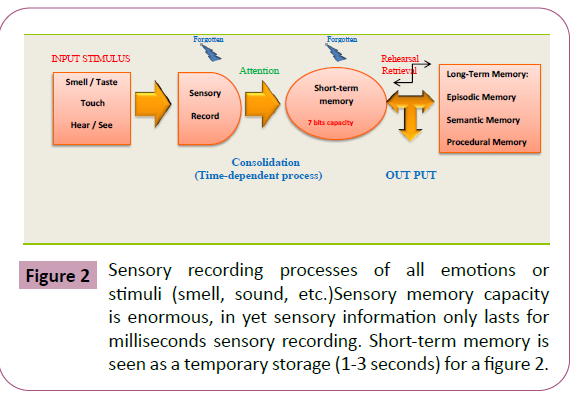
Pleasant aromas can be associated with relaxation training like diaphragmatic breathing, mindfulness training, hypnotherapy, and biofeedback. The aroma has been linked to the experience of relaxation, and in the future, exposure to this perfume or even just thinking about it can be enough to create a relaxing response. Interferences based on mindfulness and their therapeutic ways can be beneficial to our physical and mental wellbeing. Cognitive-behavioural therapy, dialectal-behavioural therapy, and mindfulness-based stress reduction are now employed. This pairing is referred to as associative learning or higher-order conditioning in cognitive-behavioural therapy and the goal is for the conditioned stimulus (the smell) to elicit the same reaction as biofeedback, breathing, or meditation [39]. Consciousness is found throughout the body and is a dynamic process that requires balance in the fluctuating membrane potentials of all cells to sustain homeostasis. Oscillating membrane potentials accompany inspiration and expiration in all cells, and they play a critical role in human subconscious awareness of feelings and states of mind. Mental imagery link with brain regulation in psychotherapy can be a new link between neuro feedback systems in networks neuromodulator for neuron-psychotherapies (depression, anxiety, and addiction) [40]. The neuro feedback system helps to facilitate mental imagery on its own. The ability of mental images to create emotional conditions is their most important feature [15]. Mood and anxiety disorders are influenced by the emotional system, and mental imagery is frequently employed to alleviate the symptoms of these diseases. Techniques that alter brain activity can be adapted to support the neurological processes that take place in these networks because mental imagery and emotion control recruit defined brain regions. Memory is a dynamic phase in the olfactory system, involving spatiotemporal oscillations in the OB and Preform Cortex (PC), which are linked to respiratory activity [41]. A pattern of Amplitude-Modulated (AM) waves is associated with memory formation [42]. These AM patterns alter with new Odour encounters and occur with each sniff of learned aromas. The onset of synaptic change is episodic and is related to nasal breathing, which is related to the function of norepinephrine [43]. In clinical situations, this interrelationship between episodic memory and mental imagery seems to be of particular importance. Some common psychopathologies are categorized through disturbing mental images of emotionallycharged past experiences, such as PTSD, they have established the main symptom [44]. From knowledge acquisition through retention, memory goes through three stages: encoding, consolidation, and retrieval. Respiration appears to have an essential part in the behavioural and neurological mechanisms connected with the encoding and recognition stages, according to animal and human research according to animal and human.
Olfactory Mental Imagery & Respiratory Function: New Pattern of Breathing
Can olfactory stimulation improve the pattern of breathing and increase the tidal volume and its depth? What makes this improved pattern possible? The first theory concerns the natural breathing pattern in the rest and relaxation position, which includes slow and deep breathing and low numbers. Because inhaling aromatic substances is linked to rest and relaxation, mental images of pleasant aromas can lead to deeper breathing and a reduction in the number of breaths by the retrieval of the autobiographical memory [20]. The second hypothesis is between the neocortical slow-wave sleep (alpha waves) oscillations and their association with respiration as a perspective of olfactory system on the cortical rhythms. The neocortical slow-wave sleep oscillations are associated with respiration [45]. Viczko J, et al. [46] in 2014 showed in the anesthetized mice by recording method multisite local field potential that respiratory-related oscillatory neural activities are probable limited to primary olfactory structures in the slow-wave of forebrain conditions. The link between breathing and neural activity in the olfactory regions and the hippocampus has recently been clearly demonstrated, its neurophysiological basis has be well assessed by the mechanical sensitivity of the olfactory epithelium. This link resonates throughout the brain and can modulate a person's behaviour and state of consciousness. In human, nasal breathing also involves the oscillating activity of the hippocampus, and memory detection rises at the peak of inhalation of the nose. These findings show for the first time that respiration has a direct effect on the integration of episodic memories, and they are added to the growing evidence that the respiratory cycle affects cognitive activity. Thus Odour receptors to the brain are the source of olfactory mental representations. Millions of sensory neurons in the Odour epithelium initiate an electrical signal that travels to the Odour Bulb (OB) at the base of the forebrain. The behavioural and physiological aspects of olfactory perception are conserved between instances of olfactory imagery, which include an individual's heart and respiratory rate, as well as sniffing behavioural (rate and volume). All of which have identical attributes in olfactory perception. For example, in the case of olfactory perception of unpleasant Odour, we shorten the breath, so the negative characteristic of Odour increases heart rate and respiration. The olfactory image of unpleasant Odours preserves these events. Neuroimaging (PET scans and fMRI) indicates that olfactory conceptual processing areas are activated in olfactory imagery and that these activations are similar to those seen in real-life olfactory perception. Olfactory perception makes us consciously aware of an Odour. Olfactory perception is strongly connected to many emotional and cognitive factors such as arousal, attention, learning and experiences [47,48]. These factors regulate both the perception of Odours and how an individual responds to those precepts is paramount for appreciating the orchestration of behavioural.
Nasal Breathing/Memory Consolidation & COVID-19
Respiration through the nose, but not through the mouth, entrains brain oscillations that improve encoding and recognition processes. Remarkably, while the link between respiration and brain activity has a long history of application to therapy, its neurophysiology has yet to be discovered. In 2018, Arcadian and et al discovered that breathing has an effect on the consolidation stage. Memory consolidation is a time-dependent process for transforming to the long-term memory that is associated by structural and chemical alterations in the nervous system (e.g., the strengthening of synaptic connections between neurons). Nasal breathing, as opposed to mouth breathing, can improve memory recognition during the consolidation stage [49]. This finding suggests that nasal breathing is firstly significant in a critical period when memories are reactivated and reinforced. Secondly, neural mechanisms can be triggered in response to nasal breathing. Nasal breathing is essential for the generation of γ oscillation in the Olfactory Bulb (OB). Nasal breathing can entrain these oscillations and lead them to the OB. The respiratory-entrainment rhythm spreads in the olfactory areas before being transported to the piriform cortex, where it is propagated in the hippocampus and medial Prefrontal Cortex (mPFC), all of which play a significant role in memory processing [50]. For memory formation, these oscillations must be regulated throughout brain processes. Mouth breathing suppresses these processes in humans, thus these rhythms and impact coding, as well as recognition processes, are eliminated, resulting in a reduction in the memory consolidation stage [49]. There are three types of oscillations in the hippocampus/prefrontal areas that are associated to memory function and are controlled by nasal breathing, according to studies by Zhuang L, et al. [51], and Joo HR, et al. [52] Sharp-Wave Ripples (SWRs). SWRs are highly synchronized fast oscillations that occur in the hippocampal formation during sleep/wake rest stages, and their rate increases rapidly because they are linked to the memory consolidation stage [51]. During consolidation our recognition memory considerably amplified through nasal breathing compared with mouth. In other words, nasal breathing directly influences on the consolidation of olfactory episodic events, and it modulates perception and cognition in humans [49]. Herrero JL, et al. [53] supported this link (respiration and brain activity), and suggested that respiration rhythms is an organizing principle of cortical oscillations in the human brain. In human, the respiration rate can be controlled volitionally by the network of areas include: caudalmedial frontal, premotor, orbitofrontal, and motor cortex, insula, superior temporal gyros, and amygdala and in attentive breathing include: anterior coagulum, premotor, insula, hippocampus. These data support the theory that the nasal respiratory cycle influences essential cognitive functioning, and the respiratory cycle pattern under coronavirus can be revised by retrieval of the episodic memory. Therapies are still used with voluntary and conscious breathing control techniques.
Aromatherapy (lung-smell) & COVID-19
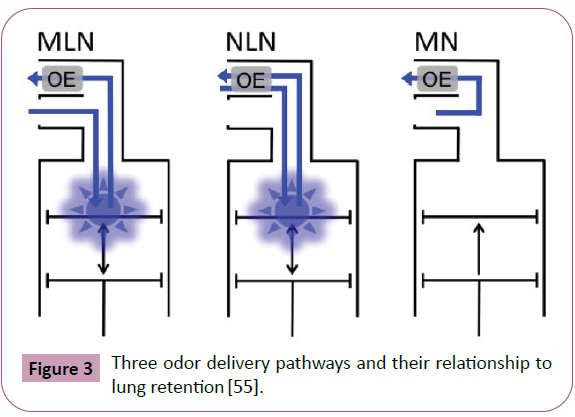
Odours usually involve the lungs on their way to the nose. The lungs serve as a sink for odours, lowering both the retro nasal odour concentration and the composition of the odour mixture. Lung retention is a basic metric for determining the efficiency of this sink. Many volatile organic compounds are considered to be retained in the lungs, which has been studied in the sense of environmental toxicology. The lungs may have a substantial effect on odour detection, according to data on human lung retention, with the intricacies of active sampling such as sniffing, smoking, and vamping influencing this. There are two modes of smell: orthonasal and retro nasal. These modalities are distinguished by the source of the odour: orthonasal draws scents inwardly via inward airflow, whereas retro nasal makes odours accessible inside via outward airflow [54]. Verhagen proposed that refinement in identifying the retro nasal smell mechanism based on the odour’s trajectory, as depicted schematically, because of the potentially considerable impact of lung retention on scents (Figure 2) [55].
OE: Olfactory Epithelium
MLN: Mouth-Lung-Nose, implying that Odorants pass through the mouth. This usually happens when you're smoking or inhaling through your mouth. Retention of the lungs is a problem.
NLN: Nose-Lung-Nose, which indicates scents enter the body through the nose. When sniffing or breathing with your lips closed during orthonasal scent, this is the most typical symptom. Retention of the lungs is a problem.
MN: The area between the mouth and the nose, where scents accumulate.
Only a few trajectories engage the retro nasal nasal cavity, despite the fact that all trajectories eventually do. The retro nasal fragrance is the most important aspect of the lungs' participation in olfaction, hence it will be prioritized. Exhalation of Odours elicits retro nasal smell, which is vital in the perception of orally generated food Odours entering the nasal cavity through the nasopalatine duct. When chewed or swallowed, oral Odorants enter the nasal cavity and exit through the nasal passages [56,57]. Lung Retention (LR) makes roughly half of the olfactory concentration retro nasal accessible, resulting in a minor shift in the Odour mixture compared to sniffing (NLN) or inhaling time (MLN). However, some organic volatiles has high lung retention of 58 present, meaning that air entering the nasal cavity via the NLN trajectory contains 58 present less Odorant than the air entering the nasal cavity via the orthonasal channel [55]. As a result, the Odour of edible food has little influence on the lungs, as seen in Figure 3 in the MN image. Organic volatiles has a high LR (58%) according to studies, implying that air entering the nasal cavity via the NLN trajectory has a 58 present lower Odorant concentration than air arriving via the orthonasal channel. Because LR changes depending on the volatile, it not only limits the number of scents available for retro nasal transduction, but it also allows you to change the composition of the scents [55]. The retro nasal aroma in the NLN pathway is thought to be not only weaker than orthonasal aroma but also fundamentally different. LR results in roughly half the concentration of aromas being available retro nasal and a minor shift in Odour mixture when compared to sniffing (NLN) or inhaling (MLN). The simple way of calculating LR is the use of physicochemical properties, and the second step entails parametrically its epithelial absorption.
Discussion
Antibiotic resistance and the advent of multidrug-resistant bacteria have necessitated the development of new drugs and alternate therapies for illnesses. Aromatic materials like Essential Oils (EOs), which are widely utilized in cosmetics, health care, conventional medicine, and the food sector today, have antibacterial/ anti-inflammatory properties that could be one of the most promising solutions to this global problem. The physiological consequences of mood, tension, and working capacity are all influenced by the sense of smell. Various fragrances altered spontaneous brain processes and cognitive capabilities, as evaluated by an electroencephalograph, according to Electrophysiological Research (EEG). According to the research, olfactory stimulus plays a crucial influence in altering cognition, mood, and social behavioural [58]. Aromatherapy is a natural technique for a person's mind, body, and spirit to heal. One of the most obvious applications of clinical aromatherapy is respiratory care. Pulmonary rehabilitation is an important aspect of respiratory care with the treatment of persons with chronic pulmonary problems since it is the most effective nonpharmacological treatment for improving health-related quality of life, reducing hospital admissions, and improving feelings of dyspnoeal and fatigue. Most pulmonary rehabilitation facilities around the world were closed during the COVID-19 pandemic. Therefore, today pulmonary rehabilitation programs can be used by tele health to present virtual pulmonary rehabilitation to patients in their homes. Researchers believe that by delivering medicine directly to the lungs, they will be able to target alveolar macrophages while also maintaining a high concentration of the medicine [59]. Aromatherapy has been utilized as a popular supplemental and alternative therapy for thousands of years in many ancient civilizations, including Egypt, China, and India [60]. Aromatherapy can associate with the olfactory images in the nerve modulation process. The contexts of mental images are determined by memory and cognitive control systems while intertwined with emotional and sensory experiences. In this study, I focused on the important highlights concerning olfactory mental imagery to investigate the relationships between lungs and aromas in the form of an active sense of smell pattern by increasing tidal volume. Air hunger occurs with an increase in the predicted medullary cortical respiratory drive (driving outcome), which is alleviated by an increase in tidal volume in the lungs, which is detected by vagal pulmonary stretch receptors. Dyspnoea is often known as "air hunger," which is a subjective sense. It's worth noting that the term "consciousness" is subjective, and so dyspnoeal is as well. Dyspnoea can be treated as a different symptom and the conscious mind can be trained to feel less dyspnoea while the underlying respiratory situation remains unchanged, because dyspnoea is a highly prevalent psychosomatic symptom. This breathing pattern is characterized by shallow, quick breaths. Instead of quiet abdominal breathing, thoracic breathing is frequently used. It's linked to tremors, palpitations, and temporary giddiness. This is frequently a symptom of severe anxiety. Dyspnoea is a subjective syndrome of varying degrees of breathing pain, is linked to interactions between a number of physiological, psychological, social, and environmental components. Psychogenic dyspnoea might be a symptom of a deeper anxiety issue. There are three common types of psychogenic dyspnoea: panic attack, psychogenic hyperventilation, and excessive sighing [61]. A dyspnoea-fear theory has been proposed, implying that the fear of dyspnoea may also trigger genuine airway obstruction in panic disorder patients [62]. With an aggravation of breathing discomfort, patients may consider breathlessness as a threat associated with anxiety or depressive symptoms, which may induce secondary physical responses. Therefore, dyspnoea may be associated with anxiety or depressive symptoms in COVID-19 patients during their hospitalization. These are anticipatory attacks and are planned ahead of time. Because most cases of dyspnoea present to family physicians, paediatricians, pulmonologists, and cardiologists rather than psychiatrists, it is critical for these doctors to be familiar with the psychosomatic dyspnoea spectrum so that a timely diagnosis can be made without unnecessary investigations and appropriate treatment can be provided. To better understand the impact of SARS-CoV-2 in the acute stage, researchers should look into the psychiatric symptoms of confirmed COVID-19 patients during their hospitalization. A thorough clinical examination, as well as a complete medical history, is required. The treatment is reassurance and sedation. Most symptoms can be effectively prevented by beta-blockers and the attack must be stopped quickly. A number of previous studies have shown a significant relationship between depressive symptoms and the stage of dyspnoea in chronic obstructive pulmonary disease (COPD) patients [63-65]. Li X, et al. [66] in 2020 showed that age and hospital stays are factors determining the rate of depression symptoms and anxiety symptoms in COVID-19 patients. Patients aged 46–60 years old also had a higher rate of depressive symptoms, and the length of hospitalization was linked to depressive symptoms. A combination of self-management programs and relaxation techniques can be useful adjuncts to psychosomatic dyspnoea treatment. Because they are frequently admitted with numerous psycho-physiological demands, symptom management of hospitalized patients with Interstitial Lung Diseases (ILDs) has been hampered by a lack of priority [67]. Aromatherapy can be a respiratory rehabilitation. Because psychological treatment is one of the components of a pulmonary rehabilitation program, and mental imagery is a key component of many mental health issues, aromatherapy may be able to help dyspnoea in both ways [68]. Therefore, aromatherapy can be an essential component in the management and maintenance of health in patients with chronic respiratory disease with a synergistic effect in standard drug therapy.
References
- Banzett RB, Pedersen SH, Schwartzstein RM (2008) The affective dimension of laboratory dyspnea: Air hunger is more unpleasant than work/effort. Am J Respir Crit Care Med 177: 1384–1390.
- Marley RA, Simon K (2007) Lung-Protective Ventilation. Annu Rev Nurs Res 35:37-53.
- Başoğlu M (2017). Effective management of breathlessness: A review of potential human rights issues. Eur Respir J 49, p.1602099.
- Peñuelas O, Keough E, López-Rodríguez L (2019) Ventilator-induced diaphragm dysfunction: Translational mechanisms lead to therapeutically alternatives in the critically ill. Intensive Care Med Exp 7: 48.
- Schmidt M, Banzett RB, Raux M. Unrecognized suffering in the ICU: Addressing dyspnea in mechanically ventilated patients. Intensive Care Med 40:1–10.
- Bellingan GJ (2002) The pulmonary physician in critical care: The pathogenesis of ALI/ARDS. Thorax 57: 540–546.
- Freeman WJ ( 2007) The place of codes in nonlinear neurodynamics. Prog Brain Res 165: 447–462.
- Phillips ME, Sachdev RN, Willhite D (2012) Respiration drives network activity and modulates synaptic and circuit processing of lateral inhibition in the olfactory bulb. Neuroscience 32: 85‐98.
- Rodriguez-Gil DJ, Bartel DL, Jaspers AW, Mobley AS, et al. (2015) Odorant receptors regulate the final glomerular coalescence of olfactory sensory neuron axons. PNAS 112: 5821-5826.
- Zelenitsky DK, Therrien F, Ridgely RC, McGee AR, Witmer LM (2011) Evolution of olfaction in non-avian theropod dinosaurs and birds. Proc R Soc B 278:3625–3634.
- Chiu A, Fischbein N, Wintermark M (2020) COVID-19-induced anosmia associated with olfactory bulb atrophy. Neuroradiology 1–2.
- Brann DH, Tsukahara PT, Weinreb C (2020) Non-neuronal expression of SARS-CoV-2 entry genes in the olfactory system suggests mechanisms underlying COVID-19-associated anosmia. Bio Rxiv.
- Holmes EA, Mathews E, Mackintosh B (2008) The causal effect of mental imagery on emotion assessed using picture-word cues. Emotion 8:395-409.
- Mathews M, Ridgeway V, Holmes EA (2013) Feels like the real thing: Imagery is both more realistic and emotional than verbal thought. Cognition and Emotion 27: 217-229.
- Moulton ST, Kosslyn SM (2009) Imagining predictions: Mental imagery as mental emulation Philosophical Transactions of the Royal Society B: Biological Sciences 364: 1273-1280.
- Renner F, Murphy FC, Ji, Manyly T (2019) Mental imagery as a “motivational amplifier” to promote activities. Behav Res Ther 114: 51-59.
- Djordjevic J, Zatorre RJ, Petrides M, Boyle JA, Jones-Gotman M (2005) Functional neuroimaging of odor imagery. Neuroimage 24: 791-801.
- Kleemann AM, Kopietz R, Albrecht J, Schopf V, Pollatos O, et al. (2009) Investigation of breathing parameters during odor perception and olfactory imagery. Chem Senses 34: 1-9.
- Rouby C, Bourgeat F, Rinck F, Poncelet J, Bensafi M (2009) Perceptual and sensorimotor differences between “good” and “poor” olfactory mental imagers. Ann NY Acad Sci 1170: 333-337.
- Masaoka Y, Sugiyama H, Katayama A, Kashiwagi M, Homma I(2012) Slow breathing and emotions associated with odor-induced autobiographical memories. Chem Senses 37: 379-388.
- Gattefossé, R.-M.Gattefossé’s Aromatherapy; C. W. Daniell Co, (1993) Ltd.: Essex, England
- De Groot AC, Schmidt E. (2016) Essential oils, Part III: Chemical composition. Dermatitis 27: 161–169.
- Koyama S, Heinbockel T. (2015) The effect of essential oils and terpenes in relation to their routes of intake and application. Int J Mol Sci 2: 1558.
- Harvey JD, Heinbockel T. (2018) Neuromodulation of synaptic transmission in the main olfactory bulb. Int J Environ Res Public Heal 15: 2194.
- Dey S, Chamero P, Pru JK, Chien MS, Ibarra-Soria X, et al. (2015) Cyclic regulation of sensory perception by a female hormone alters behavior. Cell 161: 1334–1344.
- Deshpande DA, Wang WC, McIlmoyle EL, Robinett KS, Schillinger RM, et al. (2015) Bitter taste receptors on airway smooth muscle bronchodilate by localized calcium signaling and reverse obstruction. Nat Med 16: 1299-1304.
- Aisenberg WH, Huang J, Zhu W, Rajkumar P, Cruz R, Santhanam L, et al. (2016) Defining an olfactory receptor function in airway smooth muscle cells. Sci Report 6: 38231.
- Buss D, Kudella Ph, GrüningN-M, Gisselmann G, Ständer S, et al. (2014) A synthetic sandalwood odorant induces wound-healing processes in human keratinocytes via the olfactory receptor OR2AT4. J Invest Dermato 2014; 134(11): 2823-2832.
- Kim S-H, Yoon YC, Lee AS, Kang N, Koo J, Rhyu M-R, et al.(2015) Expression of human olfactory receptor 10J5 in heart aorta, coronary artery, and endothelial cells and its functional role in angiogenesis. Biochem Biophys Res Commun 460: 404–408.
- Pluznick JL, Zou N-J, Zhang X, Yan Q, Rodriguez-Gil DJ, et al (2009) Functional expression of the olfactory signaling system in the kidney. Proc Natl Acad Sci USA 106: 2059–2064.
- Fleischer J, Bumbalo R, Bautze V, Strotmann J, Breer H (2009) Expression of odorant receptor Olfr78 in entero-endocrine cells of the colon. Cell Tissue Res 361: 697–710.
- Fukuda N, Touhara K (2006) Developmental expression patterns of testicular olfactory receptor genes during mouse spermatogenesis. Genes Cells 11: 71–81
- Parmentier M, Libert F, Schurmans S, Schimann S, Lefort A ,et al. (2009) Expression of members of the putative olfactory receptor gene family in mammalian germ cells. Nature 355: 453–455.
- Chéret J, Bertolini M, Ponce L, Lehmann J, Tsai T, et al. (2018) Olfactory receptor OR2AT4 regulates human hair growth. Nat Commun 9: 3624.
- Torabi A, Mohammadbagheri E, Dilmaghani NA (2020) Proinflammatory cykines in the olfactory mucosa result in COVID-19 induced anosmia.
- Yao L, Yi X, Pinto JM (2009) Olfactory cortex and Olfactory bulb volume alterations in patients with post-infectious Olfactory loss. Brain Imaging Behav 1: 1355–1362.
- Villemure C, Slotnick BM, Bushnell MC (2003) Effects of odors on pain perception: Deciphering the roles of emotion and attention. Pain 106: 101–108.
- Heck DH, Kozma R, Key LM (2019) The rhythm of memory: How breathing shapes memory function. J Neurophysiol 122I: 563-571.
- Jerath R, Cearley SM, Barnes VA, Junca S (2017) The Dynamic role of breathing and cellular membrane potentials in the experience of consciousness. World J Neuroscience 7: 66-81.
- Skottnik L, Linden DEJ. (2019) Mental imagery and brain regulation new links between psychotherapy and neuroscience. Front Psychiatry.
- Barrie JM, Freeman WJ, Lenhart MD (2019) Spatiotemporal analysis of prepyriform, visual, auditory, and so esthetic surface EEGs in trained rabbits. J Neurophysiology 76: 520–539.
- Freeman WJ, Schneider W (1982) Changes in spatial patterns of rabbit olfactory EEG with conditioning to odors. Psychophysiology 19: 44–56.
- Kozma R, Freeman WJ (2003) Basic principles of the KIV model, and its application to the navigation problem. J Integr Neurosis 2: 125–145.
- Hackmann A, Holmes EA (2004) Reflecting on imagery: A clinical perspective and overview of the special issue of memory on mental imagery and memory in psychopathology. Memory 12: 389-402.
- Fontanini A, Bower JM (2006) Slow-waves in the olfactory system: An olfactory perspective on cortical rhythms. Trends Neurosci 29: 429-437.
- Viczko J, Sharma AV, Pagliardini S (2014) Lack of respiratory coupling with neocortical and hippocampal slow oscillations. 19821982. J Neurosci Res 34: 3937-3946.
- Piarulli A, Zaccaro A, Laurino M (2018) Ultra-slow mechanical stimulation of olfactory epithelium modulates consciousness by slowing cerebral rhythms in humans. Scientific Reports 8(6581)
- Bensafi M, Porter J, Pouliot S, Mainland J, Johnson B, et al. (2003) Olfacto motor activity during imagery mimics that during perception. Nat Neurosci 6: 1142-1144.
- Arshamian A, Iravani B, Majid A, Lundstro ̈M JN (2018) Behavioral/Cognitive respiration modulates olfactory memory consolidation in humans. J Neurosci Res 38: 10286 –10294.
- Tort ABL, Brankačk J, Draguhn A (2018) Respiration-entrained brain rhythms are global but often overlooked. Trends Neurons 41: 189-197.
- Zhuang L, Zhang B, Qin Z.(2019) Nasal respiration is necessary for the generation of γ oscillation in the olfactory bulb. Neuroscience 2019; 398: 218-230.
- Joo HR, Frank LM (2018) The hippocampal sharp wave-ripple in memory retrieval for immediate use and consolidation. Nat Rev Neurosci 19: 744–757.
- Herrero JL, Khuvis S, Yeagle E (2018) Breathing above the brain stems: Volitional control and attention modulation in humans. J Neurophysiol 119: 145–159.
- Rozin P (1982) Taste-smell confusions” and the duality of the olfactory sense. Percept & Psychophys 31:397–401.
- Verhagen JV (2008) A role for lung retention in the sense of retronasal smell. Chemosens Percep 8: 78–84.
- Taylor AJ (1996) Volatile flavor release from foods during eating. Crit Rev Food Sci Nutr 36:765–784.
- Hodgson M, Linforth R, Taylor A (2003) Simultaneous real-time measurements of mastication, swallowing, nasal airflow, and aroma release. J Agric Food Chem 51 5052–5057.
- Sowndhararajan K, Kim S (2016) Influence of fragrances on human psychophysiological activity: With special reference to human electroencephalographic response. Sci Pharm 84: 724–752
- Labiris NR, Wabel MB (2003) Pulmonary drug delivery. Part I: Physiological factors affecting therapeutic effectiveness of aerosolized medications. Br J Clin Pharmacol 56: 588–599.
- Ali B, Al-Wabel NA, Shams (2015) Essential oils used in aromatherapy: A systemic review. Asian Pac J Trop Biomed 5: 601–611.
- Sahasrabudhe TR (2013) Psychogenic dyspnea. Medical J Dr. D. Y. Patil Vidyapeeth. 6: 14-18.
- Spinhoven P, Sterk PJ, Van Der Kamp L, Onstein EJ (1999) The complex association of pulmonary function with panic disorder: A rejoinder to Ley. J Behav Ther Exp Psychiatry 30: 341-346.
- Parshall MB, Schwartzstein RM, Adams L (2012) An official American Thoracic Society statement: Update on the mechanisms, assessment, and management of dyspnea. Am J Respir Crit Care Med 185: 435–452.
- Papaioannou A, Bartziokas K, Tsikrika S (2013) The impact of depressive symptoms on recovery and outcome of hospitalized COPD exacerbations. Eur Respir J. 41: 815–823.
- Schuler M, Wittmann M, Faller H, Schultz K (2018) The interrelations among aspects of dyspnea and symptoms of depression in COPD patients -a network analysis. J Affect Disord 240: 33-40.
- Li X, Tian J, Xu Q (2020) The associated factors of anxiety and depressive symptoms in COVID-19 patients hospitalized in Wuhan, China. Psychiatric Quarterly N.
- Zhou YH, Mak YW (2017) Psycho-Physiological associates of dyspnea in hospitalized patients with interstitial lung diseases: A cross-sectional study. Int J Environ Res Public Health 14: 1277.
- Nici L, Donner C, Wouters E (2006) American Thoracic Society/European Respiratory Society statement on pulmonary rehabilitation. Am J Respir Crit Care Med 17: 1390–413.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences