Acute Bilateral Loss of Vision by Progesterone: A Rare Case Report
Praveen kumar G1 and Mirza Mohtassam Baig2*
1Department of Anatomy, Al–Azahar Medical College, Kerala, India
2Department of Cardiology, Gleneagles Global Hospitals, Hyderabad, India
- *Corresponding Author:
- Mirza Mohtassam Baig
Department of Cardiology
Gleneagles Global Hospitals, Hyderabad, India
E-mail: drmirzamb@gmail.com
Received date: July 11, 2018; Accepted date: August 14, 2018; Published date: August 20, 2018
Citation: Kumar GP, Baig MM (2018) Acute Bilateral Loss of Vision by Progesterone: A Rare Case Report. Int J Case Rep Vol.2 No.2: 9
Copyright: © 2018 Kumar GP, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
A 35-year-old female patient was presented with acute bilateral loss of vision. The Patient recently began Progesterone treatment as prescribed by her gynaecologist for her irregular menstrual period. By the third dose, patient developed sudden loss of bilateral vision. Progesterone was discontinued and imaging studies confirmed acute bilateral optic neuritis. With methyl prednisolone treatment for 3 weeks, the vision returned to normal. Therefore, it is important that physicians should be aware of this rare but serious ocular emergency while prescribing medications.
Keywords
Progesterone; Gynaecologist; Loss of vision; Optic neuritis; Methyl prednisolone
Case Report
A 35-year-old female was brought to the emergency department by her family members after experiencing a sudden loss of vision. The emergency doctor on duty examined her. The patient had a history of irregular menstrual period since past 6 months for which she consulted a gynaecologist. After thorough examination, the gynaecologist prescribed tab Progesterone 5 mg once daily for 5 days, after taking the prescribed medicine for 3 days she experienced severe headache more at per orbital area in the second day of medication with slow progression of blurring vision. The patient stated that she was in good health without any significant history of medical conditions or surgeries, and also reported no intake of tobacco, herbal medications, and alcohol usage.
She reported that she was having continuous irregular menstrual cycle since one year for which ground work was done by gynaecologist which showed normal reports. She had been prescribed tablet Progesterone 5 mg OD for 5 days which she had taken for 3 days after which she experienced headache and blurring of vision followed by complete loss of vision.
On physical examination the patient was conscious, coherent, oriented with stable vitals, blood pressure of 120/65 mm of Hg with heart rate of 76 per min regular and temperature of 98.2°F. The other systemic examination was done which showed no abnormalities, while in the emergency department, kept a call for ophthalmologist and neurophysician on duty.
Ophthalmologist on duty examined the eyes, her pupils were normally reactive to light and demonstrated a full range of eye movements, but there was no visual activity to hand motion or figure counts.
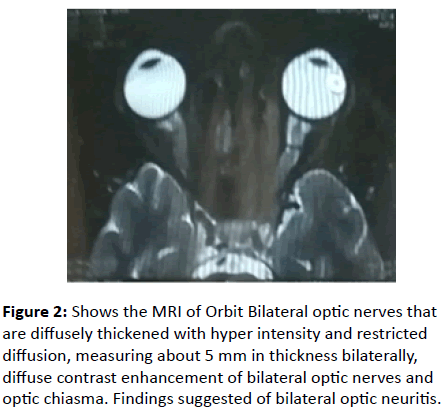
The laboratory work was done including complete blood count; blood glucose which was under normal limits. The Neurophysician on duty had examined neurologically. The speech was normal, normal strength in extremities, no facial palsies, no sensory defects. Advised a MRI Brain with Venogram thinking emboli in retinal arteries. Venogram revealed normal sinuses, he prescribed medication for migraine thinking Progesterone may cause headache and blurring vision, on the 3rd day she had experienced bilateral sudden loss of total vision (Figures 1 and 2).
Figure 2: Shows the MRI of Orbit Bilateral optic nerves that are diffusely thickened with hyper intensity and restricted diffusion, measuring about 5 mm in thickness bilaterally, diffuse contrast enhancement of bilateral optic nerves and optic chiasma. Findings suggested of bilateral optic neuritis.
Neurophysician again conducted MRI of eye ball to rule out the pathology of the optic nerve MRI of eye ball, which showed mild bulging of optic disc with acute bilateral optic neuritis with cause to rule out.
Differential Diagnosis of optic neuritis may include-Optic neuropathy by ischemia, Neuromyelitis of optic nerve, Inflammation of Optic nerve due to Infections-Syphilis and Noninfectious-like Sarcoidosis, SLE, Lyme’s disease, SLE, and due to metabolic and toxic agents causes including methanol poisoning.
The patient was admitted to the hospital, during the stay in hospital, neurologist and ophthalmologist examined her; they evaluated and revealed no anatomical or pathological causes for her loss of vision. In view of MRI of eye ball contrast showing acute bilateral optic neuritis, they have started on 1 gm of methyl prednisone IV for 3 days in the hospital and tapering dose for 3 weeks as outpatient, after 2 weeks of her medications she developed improving her vision completely, she was in complete remission in follow up visit.
Discussion
Progesterone is Norethindrone acetate which is used in hormonal contraception, hormone replacement therapy and to treat gynaecological disorders [1] such as abnormal uterine bleeding, upon oral ingestion it is rapidly converted into norethisterone by esterases during intestinal and hepatic metabolism [2] and excreted in both urine and faeces. The drug is given with precaution to the patients of cardiovascular disorders and arterial vascular disease; the progestin therapy may have adverse effects on carbohydrate [3] and lipid metabolism.
The adverse reactions observed in taking progestin’s are Changes in menstrual flow, Oedema, weight (decreases, increases), amenorrhea, Rashes, Acne, Headache/Migraine, Urticaria, Abnormalities of liver function tests may have HDL decreased and increased LDL. Thrombotic and embolic events like deep vein thrombosis, pulmonary embolism, retinal vascular thrombosis, cerebral thrombosis [4,5] and embolism, very rare Optic neuritis which may lead to complete loss of vision or partial loss.
Optic neuritis is an inflammatory disease of the optic nerve which affects young adults typically and studies show that men are less affected than women. The multiple sclerosis and optic neuritis [6] are closely related but prognosis for recovery of vision is generally good.
According to guidelines for treating optic neuritis did not exist, even though corticosteroids were used to treat the disease, but some studies demonstrate their effectiveness had not been satisfactory. The association between optic neuritis and multiple sclerosis is well established. Optic neuritis may be the first manifestation of multiple sclerosis [7], based on similarities between the two in factors as gender, age, geographic distributions, histocompatibility data, magnetic resonance imaging (MRI) changes, and family history. The risk of multiple sclerosis after optic neuritis is uncertain. The risk reported to be as low as 14 percent and as high as 85 percent. The treatment phase of the study for the Optic Neuritis Patients were randomized [8] to one of the three following treatment groups A) prednisone 1 mg/kg/day orally for 14 days, B) methiprednisolone 250 mg every 6 h through IV route for 3 days followed by oral prednisone for 11 days, C) placebo orally for 14 days.
The recovery rate of vision and visual outcome were both assessed by visual activity, colour vision contrast sensitivity, and visual field at baseline, at follow up visits during the first 3 months, and then yearly [9] neurologic examination with an assessment of multiple sclerosis status was made at baseline, after 6 months, and then yearly.
Outcome of the Treatment
The MRI eye ball has shown acute bilateral optic neuritis, patient was treated with 1 gm of methyl prednisone IV for 3 days in the hospital and tapering dose for 3 weeks as outpatient, after 2 weeks of her medications she developed improving her vision completely. She was in complete remission in follow up visit.
Follow up MRI eye ball was done after a month; there were no signs of neuritis. All the medications were stopped. Patient was advised to avoid Norethindrone acetate in future.
References
- Elks J (2014) The Dictionary of Drugs: Chemical Data: Chemical Data, Structures and Bibliographies. Springer pp: 886.
- Chwalisz K, Surrey E, Stanczyk FZ (2012) The hormonal profile of norethindrone acetate: rationale for add-back therapy with gonadotropin-releasing hormone agonists in women with endometriosis. Reprod Sci 19: 563-571.
- (1995) Venous thromboembolic disease and combined oral contraceptives: results of international multicentre case-control study. World Health Organization Collaborative Study of Cardiovascular Disease and Steroid Hormone Contraception. Lancet 346: 1575-1582.
- Lidegaard Ø, Edström B, Kreiner S (2002) Oral contraceptives and venous thromboembolism: a five-year national case-control study. Contraception 65: 187-196.
- Realini JP, Encarnacion CE, Chintapalli KN, Rees CR (1997) Oral contraceptives and venous thromboembolism: a case-control study designed to minimize detection bias. J Am Board Fam Pract 10: 315-321.
- Ramya T, Prakash B, Devi B (2014) Norethisterone induced cerebral venous sinus thrombosis (CVST): a rare case report and review of literature. Int J Reprod Contracept Obstet Gynecol 3: 231-235.
- Rajput R, Dhuan J, Agarwal S, Gahlaut PS (2008) Central venous sinus thrombosis in a young woman taking norethindrone acetate for dysfunctional uterine bleeding: case report and review of literature. J Obstet Gynaecol Can 30: 680-683.
- De Bruijn SF, Stam J, Koopman MM, Vandenbroucke JP (1998) Case-control study of risk of cerebral sinus thrombosis in oral contraceptive users and in [correction of who are] carriers of hereditary prothrombotic conditions. The Cerebral Venous Sinus Thrombosis Study Group. BMJ 316: 589-592.
- Van JG (2000) Cerebral venous thrombosis: pathogenesis, presentation and prognosis. J R Soc Med 93: 230-233.
- Piazza G (2012) Cerebral venous thrombosis. Circulation 125: 1704-1709.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences