Acute Appendicitis in Children Less Than Three Years of Age-Ultrasound, Combined with Modified Pediatric Appendicitis Score is the Most Useful Adjunct in Diagnosis
Royal Darwin Hospital, Northern Territory, Australia
- *Corresponding Author:
- Vineeth V Kumar
Royal Darwin Hospital
Northern Territory
Australia
E-mail: vinaya272@gmail.com
Received date: January 28, 2019; Accepted date: February 19, 2019; Published date: February 27, 2019
Citation: Vineeth VK (2019) Acute Appendicitis in Children Less Than Three Years of Age-Ultrasound, Combined with Modified Pediatric Appendicitis Score is the Most Useful Adjunct in Diagnosis. J Surgery Emerg Med Vol.3 No.1:23
Abstract
Aim: Appendicitis is uncommon under the age of three, with few series reported in the literature. The diagnosis has been reported to be delayed, with a perforation rate between 60-100%. The aim of this study is to delineate the presentation and outcome of appendicitis in children less than three years of age in the era of ultrasound. Methods: An investigation was carried out based on retrospective review of children under the age of three who underwent an appendicectomy over a 12-year period. Modified Pediatric Appendicitis Score (MPAS) was retrospectively applied with a score of 5 and above correlating with a high likelihood of acute appendicitis. Results: Thirty children underwent appendicectomy for acute appendicitis. The mean age was 26.4 months. Ultrasound was performed in 25 patients (83.3%) at presentation and diagnostic in 20. The remaining five patients had a high MPAS consistent with a high-likelihood of acute appendicitis. Perforation was noted in 13% of patients (n=4) and an appendicular mass was found in two patients. Ultrasound when combined with a MPAS had 100% accuracy in this population. Conclusions: In children less than three years of age ultrasound combined with the MPAS seems to be an accurate diagnostic tool in acute appendicitis, with a low incidence of perforation.
Keywords
Appendicitis; Ultrasound; Pediatric appendicitis score
Introduction
Acute appendicitis is the most common emergency presentation requiring surgical intervention in both adults and children. During 2013-2014 in Australia, almost 29,000 appendicectomies were performed, comprising approximately 10% of all emergency surgery [1]. Acute appendicitis is relatively rare in infants and becomes increasingly common in childhood and early adult life [2]. They often lack classic clinical features seen in adults. This poses a challenge for the treating physician in making a timely diagnosis [3]. It’s often a dilemma to confirm if the child is having appendicitis or not because many present with symptoms and signs that resemble other common but self-limiting causes [3].
Grading systems like the Alvarado and Samuel’s pediatric appendicitis score (PAS) have been developed to aid accurate diagnosis of appendicitis [4-7]. The PAS is a score that was first reported by Samuel in Journal of Pediatric Surgery in 2002 [5].
Ultrasound has been commonly used to diagnose appendicitis with a range of reported sensitivities (71.2-99%) and specificities (91.3-98.2%) [8-15].
Pershad et al. found that performing ultrasound on all children with suspected appendicitis was the most cost-effective diagnostic approach [16].
The purpose of this study is to analyze the use of Modified PAS combined with Ultrasound as an adjunct to aid early diagnosis of appendicitis in children below three years of age.
Patients and Methods
The study was a retrospective analysis of children below 3 years of age who underwent appendicectomy over a period of 12 years at a tertiary Australian children’s hospital between May 2005 and August 2017. Ethics approval was granted by the hospital Human Research and Ethics Committee.
Patients
The study involved 82 children below 3 years of age who underwent Appendicectomy in a span of 12 years. About 52 patients were excluded from the study, as they had undergone opportunistic appendicectomy whilst been operated for various other reasons like obstruction of bowel, intussusceptions, diaphragmatic hernia repair and gastrointestinal infections such as gastroschisis. Thirty patients were included in the study, who were diagnosed with AA supported with post operative histological diagnosis.
Methods
Clinical signs and symptoms: Clinical diagnosis of AA was determined by the treating Pediatric surgeon and the presentation of acute abdomen was recorded. The clinical history of right lower quadrant pain, vomiting, fever, anorexia, irritability with associated signs of percussion and rebound tenderness in the right lower quadrant of the abdomen, and cough tenderness was considered.
Since PAS score is usually used in children aged 4 to 15 years, we modified the score to include children under 3 years of age. Modifications included changes from anorexia to poor feeding or loss of appetite in infants and only pain instead of migratory symptoms of pain was considered. MPAS score calculated which included the following criteria mentioned in Table 1 below.
Table 1 Modified Pediatric appendicitis score includes the following criteria.
| Parameter | Score |
|---|---|
| Loss of appetite/Poor feeding | 1 |
| Nausea/emesis | 1 |
| Fever | 1 |
| Pain | 1 |
| Tenderness in right lower quadrant | 2 |
| Cough/percussion/hop tenderness | 2 |
| Leucocytosis | 1 |
| Neutrophilia | 1 |
| Total | 10 |
MPAS of less than 5 was considered unlikely, and that of 5 and above was considered most likely for appendicitis. MPAS score was applied to all the children included in our study.
Laboratory tests: Blood tests for Leucocyte and differential count, C-receptive protein were defined, depending on the age of the child [17]. These investigations were done as per the protocols prevailing in our hospital.
Histologically proven appendicitis was considered as the gold standard for our study. Histopathology reports of the appendix from those who underwent surgery were collected in order to confirm the diagnosis of appendicitis.
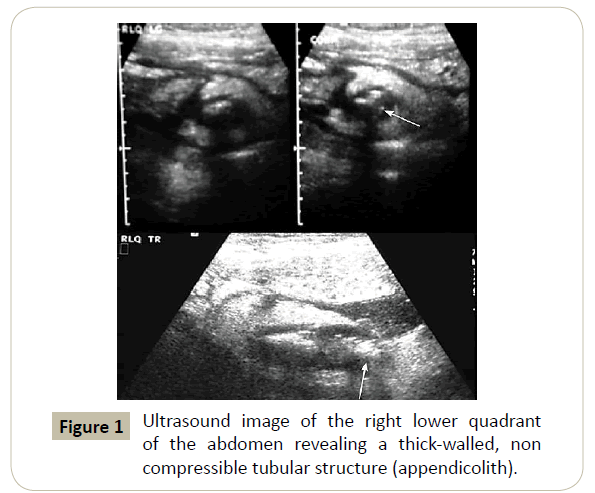
Ultrasonography: It was not done in children with apparent clinical indications of diffuse peritonitis and evident signs of peritonism to avoid delay in surgical management. Radiological diagnosis of AA was made by an accomplished sonologists. It depended on the accompanying criteria: representation of a non-compressible, aperistaltic, maximal outside diameter (MOD) diameter of more than 6 mm, using a graded compression technique giving an "objective like" cross-sectional perspective and a tubular appearing structure, encompassed by echogenic-aroused fat. Other features of hyperemia, presence of appendicolith, and the absence of gas in the lumen, free peritoneal fluid in the pelvis or right iliac fossa was considered sonographically diagnostic for appendicitis. Sonographic appearances similar to those shown in Figure 1 were confirmed to be diagnostic for appendicitis.
Statistical analysis: Data were presented as mean and range for numeric data and as prop oration where is possible for categorical data. The data was also subjected for statistical analysis using an unpaired t test. Sensitivity, specificity, predictive values, and diagnostic accuracy of ultrasonography and of clinical signs were calculated using Bayes’ theorem. The differences were considered to be statistically significant when P values were lower than 0.05.
Results
The female to male proportion was about 1:1.5 in the children in the study (Table 2). The mean age of children was below three years. More than 80% of children showed symptoms of abdominal pain, fever, vomiting and tenderness; some of children also showed anorexia and diarrhea (Table 3). The mean WCC was 16.2 × 103 cells per litre. The CRP was 132.2 mg/L (Table 4).
Table 2 Demographic characteristics.
| Characteristic | Value |
|---|---|
| Number of patients | 30 |
| Mean age in years ±SD | 2.27 ± 0.57 |
| Sex (Male and Female) (%) | 38.7 and 61.3 |
Table 3 Symptoms observed in the patients.
| Symptom | No symptom (%) | Symptoms observed (%) |
|---|---|---|
| Pain | 12.9 | 83.9 |
| Nausea | 61.3 | 35.5 |
| Vomiting | 6.5 | 90.3 |
| Fever | 6.5 | 90.3 |
| Loss of appetite/Poor feeding | 32.3 | 64.5 |
| Diarrhea | 77.4 | 19.4 |
| Tender | 12.9 | 83.9 |
| Distention | 77.4 | 19.4 |
Table 4 Diagnostic results of the children.
| Laboratory Test | Positive |
|---|---|
| WCC (x103Cells/L) | 16.02 ± 1 5.1 |
| CRP (mg/L) | 132.2 ± 71.9 |
Abdominal ultrasound was performed in 25 out of 30 (83.3%) of patients. 5 patients has a high MPAS score of more than 5 and were unwell and hence an abdominal ultrasound was not performed and underwent surgery immediately. USS was diagnostic for AA in 20 (80%) children. Appendicular mass were identified in 2 patients and perforation of the appendix was diagnostic in 4 (13%) (Table 5).
Table 5 Abdominal Ultrasound findings.
| USS done | Positive | Not diagnostic | Not done |
|---|---|---|---|
| n=25 (83.5%) | 20 (80%) | 5 | 5 |
| Perforation | 4 (13%) | ||
| Appendicular mass | 2 |
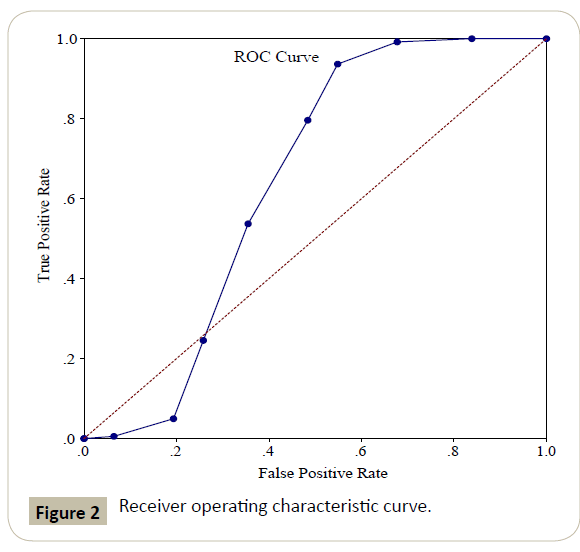
An receiver operating characteristic (ROC) curve (Figure 2) was constructed to assess MPAS and performance in the population tested. The outcome yielded an area under the curve of 0.6393. The best cut-point, calculated to maximize the sensitivity and specificity and found at specificity, potential negative appendectomy rate, and missed appendicitis rate were calculated. No other single cut-point offered an improved sensitivity and specificity.
Discussion
The investigation of AA in children is evaluated and compared from clinical view. The clinical findings including laboratory tests and ultrasonographic outcome were compared.
ROC were used to evaluate how precisely restorative analytic tests can segregate between two patient states i.e., disease vs. non-disease. A ROC curve depends on the principle of ‘separator’ scale, on which comes about for the infected and non-diseased structure a couple of covering conveyances [18]. The complete separation of the two underlying distributions suggests a segregating test while complete overlap implies no discrimination. In the current investigation, the ROC curve shows the trade-off between the true positive rate and false positive rate indicating the validity of the method employed.
In our study, the abdominal ultrasound demonstrated the high accuracy, specificity and, positive prescient findings. In contrast to the outcomes, the most noteworthy sensitivities and negative prescient values were accomplished by white blood cells and CRP which were elevated. Similar clinical findings such as ultrasonography and routine laboratory tests (leucocytes count and C-receptive protein) and clinical findings were reported in adults [5,19,20]. The clinical signs had the highest sensitivity, specificity and positive predictive value. A comparative affectability, however much higher specificity of clinical findings was found in a Dutch study [21].
In our study, abdominal ultrasound in 80% (observed in 20 children) were diagnostic for acute appendicitis and identified perforation in 13% and appendicular mass in 6% of patients (Table 4). These findings indicate that USS is sensitive method in diagnosis of acute appendicitis. Due to high sensitivity in terms of diagnosis of appendicitis, the use of abdominal ultrasound was considered as an essential diagnostic modality in numerous studies [7]. In this study we found that the better predictability of ultrasound in children for the diagnosis of AA. The abdominal ultrasound combined with modified appendicitis score had almost 100% accuracy and higher probability in identifying perforation and appendicular masses in this pediatric age group.
Limitations
Unfortunately, USS is in its poor predictability in comparison to CT scan making the method-limited use for diagnosis. The inverse is valid for CT examines, where intraperitoneal fat really enhances the predictability for appendicitis. Technical viewpoints influencing the capacity of the sonographer to accomplish sufficient pressure of the RLQ i.e., obesity, extreme agony or abdominal guarding, excess bowel gas and an uncooperative patient can all influence the accuracy of the ultrasound. In case of appendicitis related to retrocecal segment, it is quite hard to recognize as high-recurrence transducers might fail to find the profound structures. Operator experience can likewise influence the study result. A perforated appendix can bring about an uncertain or false negative study. This is likely in cases of severe guarding in patient with peritonitis.
Conclusions
We believe that the combination of clinical findings and calculating MPAS along with an abdominal ultrasound in children less than three years of age seems to be an accurate diagnostic tool in acute appendicitis and could help clinicians to prevent any delayed diagnosis appendicular mass formation or perforation.
References
- Australian Institute of Health and Welfare (2015) Admitted Patient Care 2013-14: Australian Hospital Statistics. Health services series no. 60. Cat. no. HSE 156. AIHW, Canberra, Australia.
- Williams N, Bulstrode CO, Connell P (2013) The Vermiform appendix. In: O’ Connell PR (ed.) Bailey and Love: Short practice of Surgery. (26thedn), New York: CRC Press 013: 1199-1200.
- Mason JD (1996) The evaluation of acute abdominal pain in children. Emerg Med Clin North Am 14: 629-643.
- Eriksson S, Granstrom L, Carlstrom A (1994) The diagnostic value or repetitive peroperative analyses of C-reactive protein and total leucocyte count in patients with suspected acute appendicitis. Scand J Gastroenterol 29: 1145-1149.
- Eriksson S, Granstrom L, Olander B, Wretlind B (1995) Sensitivity of interleukin-6 and C-reactive protein concentrations in the diagnosis of acute appendicitis. Eur J Surg 161: 41-45.
- Gaitini D (2011) Imaging Acute Appendicitis: State of the Art. J Clin Imaging Sci 1: 49.
- Gaitini D, Beck-Razi N, Mor-Yosef D, Fischer D, Ben Itzhak O, et al. (2008) Diagnosing acute appendicitis in adults: accuracy of color Doppler sonography and MDCT compared with surgery and clinical follow-up. AJR Am J Roentgenol 190: 1300-1306.
- Sivit CJ, Applegate KE, Stallion A, Dudgeon DL, Salvator A, et al. (2000) Imaging evaluation of suspected appendicitis in a pediatric population. Am J Roentgenol 175: 977-980.
- Wiersma F, Toorenvliet BRB, Bloem JJL, Allema JH, Holscher HC (2009) US examination of the appendix in children with suspected appendicitis: the additional value of secondary signs. Eur Radiol 19: 455-461.
- Gracey D, McClure MJ (2007) The impact of ultrasound in suspected acute appendicitis. Clin Radiol 62: 573-578.
- Baldisserotto M, Marchiori E (2000) Accuracy of non compressive sonography of children with appendicitis according to the potential positions of the appendix. AJR Am J Roentgenol 175: 1387-1392.
- Dilley A, Wesson D, Munden M, Hicks J, Brandt M, et al. (2001) The impact of ultrasound examinations on the management of children with suspected appendicitis: a 3-year analysis. J Pediatr Surg 36: 303-308.
- Limchareon S, Wongsuttilert A, Boonyarit A (2014) Efficacy of ultrasonography in evaluation of suspected appendicitis in pediatric population. J Med Ultrasound 22: 213-217.
- Mittal MK, Dayan PS, Macias CG, Bachur RG, Bennett J, et al. (2013) Performance of ultrasound in the diagnosis of appendicitis in children in a multicenter cohort. Acad Emerg Med 20: 697-702.
- Puylaert JB (1986) Acute appendicitis: US evaluation using graded compression. Radiology 158: 355-360.
- Pershad J, Waters TM, Langham MR, Li T, Huang EY (2015) Cost-effectiveness of diagnostic approaches to suspected appendicitis in children. J Am Coll Surg 220: 738-746.
- Engorn B, Flerlage J (2015) Haematology. In The John Hopkins Hospital, The Harriet lane Handbook. Philadelphia, Elsevier Saunders 14: 314.
- Swets JA (1979) ROC analysis applied to the evaluation of medical imaging techniques. Invest Radiol 14: 109-121.
- Tepel J, Sommerfeld A, Klomp HJ, Kapischke M, Eggert A, et al. (2004) Prospective evaluation of diagnostic modalities in suspected acute appendicitis. Langenbecks Arch Surg 389: 219-224.
- Al-Rasheed A (2012) Elevation of white blood cells and platelet counts in patients having chronic periodontitis. Saudi Dent J 24: 17-21.
- Van den EED, Boellaard WP, Allema JH, Holscher HC, Putter H, et al. (2003) Diagnostic surplus value of echography in children with acute abdominal pain. Ned Tijdschr Geneeskd 147: 1174-1177.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences