ISSN : 2576-3911
Integrative Journal of Global Health
Active Engagement of Community Stakeholders and their Capacity Building for Better Hygiene Practices in Tribal Odisha, India: A Case of Balasore District
Subham Chirania1 and Abhijeet Sinha2*
1Swaniti Initiative, New Delhi, Delhi, India
2India Manager-USLP, Hindustan Unilever Limited, Mumbai, Maharashtra, India
- *Corresponding Author:
- Abhijeet Sinha
India Manager-USLP
Hindustan Unilever Limited, Unilever
Sustainable Living Plan, Mumbai
Maharashtra, India
Tel: 8294638242 E-mail: abhijeetpsinha@gmail.com
Received date: February 08, 2017; Accepted date: February 20, 2017; Published date: March 02, 2017
Citation: Chirania S, Sinha A. Active Engagement of Community Stakeholders and their Capacity Building for Better Hygiene Practices in Tribal Odisha, India:A Case of Balasore District. Integr J Glob Health. 2017, 1:1.
Abstract
A comprehensive study was undertaken in a tribal community of Odisha, India to improve health outcome indicators by promoting access to better personal hygiene and sanitation. The approach embraced a community-based, actionoriented model for social change in which an integrated strategy was designed to improve health and hygiene in the community. The strategy was implemented with active participation of key stakeholders within the community using Capacity Building Model. A questionnaire was designed and used before and three months after the intervention. The effect of the intervention was evaluated by measuring behavior changes in the population towards personal hygiene. Statistically significant changes were observed in behavior of the population with regards to use of toilet and soap. A chi-square test of independence was performed to examine the relation between community-led interventions and behavior change after three months of the intervention. The relation between these variables was significant, χ2 (2, N=136)=31.373, p<0.01.
Keywords
Capacity building model; Community; Active participation; Hygienic behavior; Health
Introduction
While India is a fast developing economy, hundreds of millions of people in the country are still impoverished. The Planning Commission of India in 2011-12, following the Tendulkar Committee Methodology1, estimated that 270 million Indians (or 21.9% of the total population) were living Below Poverty Line (BPL). Further, the Committee ranked Odisha at sixth position in the list of all states, declaring 32.6% of the total state population as BPL. Such huge levels of poverty also reflected on the health indicators of the state. The Infant Mortality Rate2 (SRS 2013) and Maternal Mortality Rate3 (SRS 2010-12) in Odisha were 51 and 235 respectively, much higher than the national average (IMR: 40, MMR: 178). These figures also substantiated other research studies, which state that poverty and ill-health are closely intertwined [1]. In this context, it particularly becomes important to focus on improving health outcome indicators to evade from the vicious cycle of ill-health and poverty.
The present study was carried out in Kalika, a tribal GP (Gram Panchayat) under Jaleswar Block in Balasore district of Odisha. Kalika has a significant number of BPL households. As per a 2011 survey conducted by the Block Program Unit of the Odisha Livelihood Mission, out of 1,319 households in Kalika, 488 (or 37%) households were classified as Poor and 37 (or 3%) households were categorized as EPVG (Extremely Poor and Vulnerable Group). In the recent past, the GP also reported multiple instances of Infant deaths, Malnutrition and various morbidities, particularly among children. From June’16 to August’16, Jaleswar alone reported 15 cases of Severe Acute Malnutrition (SAM) out of 42 total cases registered in Nutrition Rehabilitation Center (NRC), Balasore.
In 2015, Kalika was identified for transformation into a Model Village under a flagship rural development scheme of the Government of India. As part of this project, one of the researchers worked directly with the office of MP (Member of Parliament) Lok Sabha, Balasore to design a development framework for Kalika such that it gets transformed into a model for other villages to emulate. The timeline for the project was 10 months. Apart from infrastructure development, the approach focused more on developing coalition of community institutions and individuals to combat challenging problems [2] and encouraging community involvement in problem-solving strategies such that individuals within the community gain confidence and vision to work for positive changes in their lives, individually and together with others, once the external support was withdrawn. This research therefore focuses on the concept of “Working with People”, an approach for rural development in which projects have to be developed by people with an active role instead of for people [3].
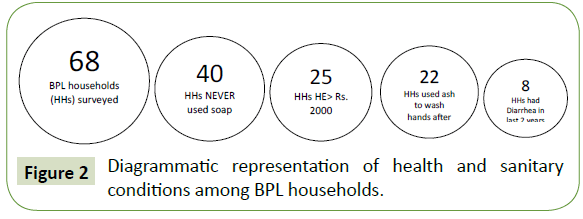
The health services and infrastructure in Kalika were in a dilapidated state and demanded immediate attention. For a preliminary assessment of the health and hygiene situation in Kalika, as the first step, the researchers facilitated health checkup of 30 people, selected randomly, by an external medical practitioner. The idea was to get an unbiased report on current health scenario of the GP. The medical examination revealed that most of the health ailments in the GP, particularly among women and children, were due to lack of proper hygiene and sanitation. Most women were found to have low Body Mass Index (BMI) and many suffered from anemia and urine infections. Diseases such as malaria and diarrhea were a common phenomenon. For further assessment, the researchers visited the Schools and Anganwadi Centers (AWCs)4 in the GP. Most of the schools and AWCs did not have proper toilet facility and many children were seen defecating and urinating openly in the school premises. Moreover, the children did not wash hands after defecation and this was due to lack of any dedicated hand-washing space. Interaction with women and frontline workers also revealed that many women and adolescent girls, particularly those belonging to the BPL category, practiced poor menstrual hygiene. It was also noticed that despite more than 95% households in Kalika had built a toilet under Swachh Bharat Mission, many people continued to defecate in the open. Health concerns as a result of poor hygiene practices, as stated further in the Results section, also added to the health expenditure of households (Figure 2).
The above observations highlighted the need to carry out some intervention engaging the key stakeholders of the community for a long term behavior change. The present study aimed to examine causes behind poor hygiene behavior and design appropriate intervention approach to improve the same for better health outcomes.
Methodology
The methodology adopted in this study was based on structured observation and situational assessment through household interviews. The researchers initially visited the schools, AWCs and hospital to observe and understand the health services and hygiene facilities. Later a comprehensive survey was undertaken for detailed understanding of health and hygiene at household level.
Post survey, the intervention methodology was based on Community Participation [4]. This was done through participatory planning with all stakeholders (frontline health workers, in this case) involved in the project, right from its formulation and implementation phases to ensuring its sustainability through future management. Frontline workers (FLWs) include ASHAs5 (Accredited Social Health Activists), AWWs6 (Anganwadi Workers) and ANM7 (Auxiliary Nurse Midwife) who serve as frontline health care professionals.
Participants
To assess the status of personal health and hygiene, a baseline survey of 136 households in Kalika was taken. Stratified data sampling technique ensured representation of households from both BPL and APL (Above Poverty Line) category in roughly the same proportion as the population under study. Out of the total 1402 households (APL=780; BPL=622), roughly 11% (68 households) of total BPL and 9% (68 households) of total APL households were surveyed. The distinction between APL and BPL households was drawn to study if the financial status of households creates any difference in health outcome and hygiene behavior.
Research measure
A semi-structured interview questionnaire was designed for the purpose of data collection. Apart from the demographics, the survey included questions related to health and hygiene background of the respondents such as material used to wash hands (soap/mud/ash), occasions on which they used soap (after visiting toilet, before or after meal, or during bathing), physical condition of hand-washing location (if any) at home, awareness regarding benefits of using soap, distance to nearest water source, availability of toilet at home, cases of malaria/diarrhea in last two years, average family health expenditure in last one year, and knowledge of any health related awareness program in last five years. There was no distinction made on the basis of caste or religion of the respondents.
Research design
Participants were interviewed before and three months after the intervention for the purpose of data analysis using the pre-post research method design.
Process of implementation
The pre-intervention survey results, as explained further in the Results section, clearly highlighted that there was a need to bridge the knowledge gap in tribal community in order to introduce behavior change. The aim of the program was to reach out to each and every individual in the village and for a successful intervention, it was imperative that the community capacity was adequately tapped and stakeholders from the community were actively involved in strategy design and implementation.
Community Capacity is the interaction of human capital, organizational resources, and social capital existing within a given community that can be leveraged to solve collective problems and improve or maintain the well-being of that community. It may operate through informal social processes and/or organized efforts by individuals, organizations, and social networks that exist among them and between them and the larger systems of which the community is a part [5]. The frontline workers in the village who interacted with households on a daily basis were subsequently identified as key resources that could help strengthen the program.
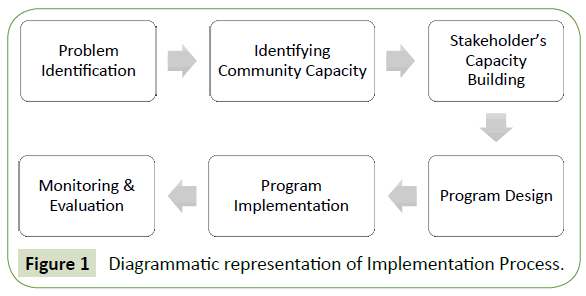
The intervention approach adopted the capacity building model [6] wherein key stakeholders such as ASHAs and AWWs were mobilized and trained to disseminate the importance of good personal hygiene and adopting regular hand wash practice. The Capacity Building Model can be characterized as the approach to community development that raises people's knowledge, awareness and skills to use their own capacity such that they are able to take decisions and communicate more effectively at different levels, eventually instilling in them a sense of confidence to manage their own destinies [7].
It was noted that while these health workers interacted with households and provided maternal and child care services as part of their daily job, they mostly worked in silos without any common objective, clearly lacked any focus and offered poor quality services (e.g., there were 2 cases of Severe Acute Malnutrition in the village that were identified only during this campaign) leading to poorer health outcomes. The lead researcher therefore took the role of a facilitator and entrusted the group of frontline health workers to lead the campaign, right from its conceptualization and designing timelines to its implementation and ensuring future success. Also, based on past experience, it was well known that a knowledge session alone might not interest the tribal community and may fail to create the desired impact. To ensure individual participation and adoption of better hygienic practices, it was decided to give two soap bars to each household that participated in the campaign. A leading soap manufacturer in the country pitched in to support this program.
After their own training, the health workers planned a series of awareness sessions in each habitation of the village over the course of next one month. The idea was to have participatory discussions in small groups rather than gathering thousands of people at once. The Schools and AWCs were identified as venues for each camp, so that women and children could easily participate. Typically, before any session, the AWW and ASHA worker of the region spread word about the schedule of the camp. The importance of using toilets, soap (at critical occasions) and good menstrual hygiene on health outcomes was extensively discussed in each meeting. School children were amused with cartoon characters to encourage them to use toilet and soap regularly, particularly after toilet and before having any meal. The school teachers were actively involved in this process and were encouraged to promote and monitor better hygiene practices in the school premises. The health workers also demonstrated Six-steps hand-washing technique, a process recommended by World Health Organization, in each of the sessions.
To prevent open defecation, peer pressure [8] was adopted as a means to encourage people to use toilets. Individuals from within the community were encouraged to prevent people from defecating in the open and introduce positive behavior change through verbal peer persuasion [9]. In some cases, the village leaders also threatened to report such cases to the law and cancel social security benefits of people found defecating in open (Figure 1).
Results
Pre intervention
Hygiene status: Out of the 136 households surveyed, 54 did not have soap at their homes. This included 14 households from APL and 40 from BPL category. While 33 out of 40 BPL households used mud or ash on a few occasions, 7 households (10% of BPLs surveyed) were neither using soap nor mud/ash. 22 BPL and 4 APL households were using ash/mud instead of soap even after defecation.
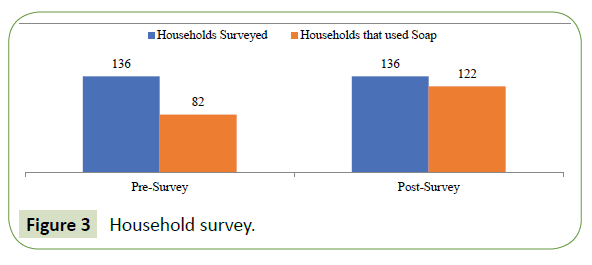
While 82 out of 136 households used soap to wash hands, it was noted that the hand-washing location in many households was too filthy and there was a highly irregular pattern of soap usage.
Knowledge gap: Out of 68 BPLs surveyed, only 45 (including ones that used soap and those that did not) said that hand hygiene is related to better health. Even among APL households, 8 out of 68 did not believe that hand hygiene results in better health.
Health expenditure: Out of the 40 BPL households that did not use soap, 25 said that their average annual health expenditure (HE) was greater than Rs. 2000 (mainly due to cases of diarrhea, pneumonia, malaria and typhoid). Moreover, 8 out of these 40 households reported cases of diarrhea in children below 5 in the past two years. On the contrary, out of 82 households those were found using soap, only 8 reported diarrhea cases in children below 5 years.
Observational survey: Structured observation carried out in Schools revealed that children washed hands neither after defecation nor before having meal. Similarly, the AWCs did not give any importance to hand hygiene of women and children and there was no soap in any of the AWCs (Figure 2).
Post intervention
The post intervention behavior interview was conducted three months after the awareness campaign to see if the households continued to use soaps, as it was assumed that in three months the two bars donated earlier would have exhausted. This household survey was conducted before 8 AM to check if people were washing their hands with soap after defecation or not. 136 households were chosen randomly for the survey this time out of which 122 households (including APL and BPL) were found using soap as compared with 82 households that were found using soap before the intervention (Figure 3).
An observational survey was also conducted in all Schools three months later and it was seen that children did wash hands with soap before their Mid-day-Meal. Women and children in AWCs were also found using soap before meal. Also, the ASHAs were seen carrying liquid hand wash during household visits to make those households wash hands that were not using soap yet. Moreover, four months after the program the researchers observed that frontline workers had planned another series of hygiene awareness program in schools to maintain the momentum and encourage children to use toilet and soap regularly.
Reporting the results of a chi-square test of independence
A chi-square test of independence was performed to examine the relation between hand wash awareness sessions and behavior change after 3 months of the campaign. The relation between these variables was significant, χ2 (2, N=136)=31.373, p<0.01 (Table 1). The statistical analysis revealed that there was a significant increase in the number of the households (including both APL and BPL) that purchased soap to wash hands post the hand wash campaign.
| χ2Calculations | Number of households that use soap | Number of households that did not use soap | Total |
|---|---|---|---|
| After Intervention | 122 | 14 | 136 |
| Before Intervention | 82 | 54 | 136 |
| Total | 204 | 68 | 272 |
χ2= 31.373, df = 1, χ2/df = 31.37, P (χ2>31.373) = 0.0000
Table 1: Two-way Contingency Table for χ2 calculations
Discussion
The study aimed to assess the impact of community stakeholders in promoting good hygienic practices at the household level in a tribal community of Odisha. Based on comprehensive evaluation of existing health and sanitary conditions, it was understood that poor hygienic practices were largely responsible for poor health outcomes in the village. Subsequently, a strategy was designed to improve personal hygiene by promoting regular use of soap [10] and toilet.
An equal sample of APL and BPL households was surveyed and it was found that 21% of APLs and 60% of BPLs did not use soap. Further investigation revealed that financial gap was not really the primary factor that governed good hygienic behavior rather it was lack of awareness and understanding that did. Moreover, households that were not found using soap reported more cases of diarrhea and greater expenditure owing to health related concerns. A medical examination of a small sample also disclosed that most health problems in the village were a result of poor hygienic behavior. The status of health services in the village was even poorer as frontline workers were unable to discharge their duties effectively and exhibited poor knowledge about health, hygiene and relevant government schemes.
A capacity building model was adopted to introduce sustainable behavior changes in the population. The capacity of health workers within the community was adequately leveraged and they were trained to lead a campaign for better health and hygiene. A series of hand-wash campaign was organized over a period of one month at key locations in the village to ensure 100% coverage of households. Benefits of hand hygiene and use of toilet were emphasized through focused group discussions in each session. Two bars of soap were also given to each household to ensure theoretical knowledge was put to practical application. The community’s response to the campaign also raised the confidence of health workers who showed greater sincerity and commitment after the campaign to ensure that households maintained good personal hygiene. A post assessment of households after three months of intervention showed that the difference in number of households using soap before and after intervention was statistically significant.
While community-led interventions have proven to be effective in the past such as decline in risk behavior and sexually transmitted infection prevalence among sex workers in Mysore, India [11], the present study supports the findings that challenging issues in rural terrains can be tackled when the community is mobilized and its capacity is adequately tapped and utilized.
This study also substantiates that there is a high positive correlation between poverty and counterproductive behavior; an observation also supported by the findings of the research ‘Poverty impedes cognitive functions’ [12]. The lack of awareness in households and the ignorance in frontline workers in Kalika made them behave in even less capable ways that further added to the misery of people and perpetuated poverty.
Limitations of the study and future research
One of the major limitations of the study was the high number of socially desirable responses to several questions which could not be included in the qualitative analysis. Variables such as households’ monthly expenditure on alcohol, infection cases among adolescent girls and women, and whether food items received at AWCs are consumed by women and children only, etc. could not be collected due to largely incorrect responses (most women were embarrassed and many were seen to be intimated by their men to answer correctly to such questions) which were recorded in initial few surveys and thus were dropped in the later stage. However, including the above variables (by establishing trust between the researcher and the community members in form of participatory action research) could have brought more clarity about fundamental issues at the grass-root level that could be related to poor health and hygiene.
Further research can include more qualitative variables for a better and more comprehensive understanding of behavior pattern in tribal communities and could be conducted over a longer period of time to study the impact of better hygiene on health indicators. Additionally, further research could help identify appropriate settings and optimal roles for community stakeholders that could result in incremental benefit from their contribution.
Conclusion
This paper examines the application of capacity building and community participation ideas in the context of health and hygiene sector in rural India. The frontline workers at the grassroot level were mobilized, trained and encouraged to implement a health and hygiene improvement strategy in a tribal community of Odisha. A number of sessions and focused group discussions were held across the village over a period of one month where benefits of good personal hygiene were emphasized. The health workers efficiently conducted the program and monitored its effective implementation. A pre-post research measure was designed and the statistical significance of behavior changes was estimated using chi-square. Significant behavior change was observed in the community three months after the intervention as most households were seen adopting better hygienic practices. The post-intervention survey showed that 90% of households in the village were using soap, school children washed hands with soap before mid-day-meal and frontline workers made it a point that women and children regularly washed hands with soap. The success of this intervention also establishes grounds for further research that could investigate appropriate settings for community stakeholders and develop management models of community participation such that they could lead to better health outcomes in rural terrains.
1The Tendulkar Committee calculated the poverty line on per capita per month basis and the line varied from State to State because of inter-state price differentials. The national average was estimated as Rs. 816 in rural areas and Rs. 1,000 in urban areas. In Odisha, the poverty line was estimated at Rs. 695 and Rs. 861 in rural and urban areas respectively. Those earning below these limits were categorized as BPL and others were categorized as APL.
2IMR = (Number of Infant Deaths (less than 1 year of age) / Number of live births during reference period) *1000
3MMR = Proportion of maternal deaths per 100,000 women in the ages 15 - 49
4Anganwadi Centers provide pre-education to children aged 3-6 years and health care support to pregnant women and mothers of children in the age group 0-6 years
5ASHAs are community health workers who create awareness on health and hygiene and mobilize the community towards local health planning and increased utilization of existing health services.
6AWWs provide care for newborn babies such as immunization, and also antenatal and post-natal care services.
7ANM is a village-level female health worker in India and is a trained medical practitioner. ANM acts as a resource person for the training of ASHAs and each ANM is supported by four or five ASHAs. ANM’s role is critical to achieving the targets of National Health Programmes in India.
References
- Wagstaff A (2002) Poverty and health sector inequalities. Bulletin of the World Health Organization, pp: 97-105.
- Butterfoss FD, Goodman RM,Wandersman A (1993) Community coalitions for prevention and health promotion. Health Education Research 8: 315-330.
- Cazorla A, Ríos I, Hernández D,Yague JL (2010) Working with people: rural development project with Aymaras Communities of Peru. In International Conference on Agricultural Engineering-AgEng 2010: towards environmental technologies, Clermont-Ferrand, France.
- Preston R, Waugh H, Taylor J, Larkins S (2009) The benefits of community participation in rural health service development: where is the evidence? National Rural Health Conference Proceedings.
- Chaskin RJ (2001) Building community capacity. Transaction Publishers.
- Eade D (1997) Capacity-building: An approach to people-centered development. Oxfam.
- Schuftan C (1996) The community development dilemma: what is really empowering? Community Development Journal 31: 260-264.
- Turner G, Shepherd J (1999) A method in search of a theory: peer education and health promotion. Health Education Research 14: 235-247.
- Smith LKC, Fowler SA(1984) Positive peer pressure: The effects of peer monitoring on children's disruptive behavior. Journal of Applied Behavior Analysis 17: 213-227.
- Curtis V,Cairncross S (2003) Effect of washing hands with soap on diarrhoea risk in the community: a systematic review. The Lancet Infectious Diseases 3: 275-281.
- Reza-Paul S, Beattie T, Syed HUR, VenuKumar KT, Venugopal MS, et al.(2008) Declines in risk behaviour and sexually transmitted infection prevalence following a community-led HIV preventive intervention among female sex workers in Mysore, India. AIDS 22: S91-S100.
- Mani A, Mullainathan S, Shafir E, Zhao J (2013) Poverty impedes cognitive function. Science 341: 976-980.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences