ISSN : 2576-392X
Dentistry and Craniofacial Research
Accelerated Orthodontics–An overview
Unnam D1, Singaraju GS1, Mandava P1*, Reddy GV1, Mallineni SK2 and Nuvvula S2
1Department of Orthodontics, Narayana Dental College and Hospital, Nellore, Andhra Pradesh, India
2Department of Pedodontics, Narayana Dental College and Hospital, Nellore, Andhra Pradesh, India
- *Corresponding Author:
- Mandava P
Department of Orthodontics, Narayana Dental College and Hospital, Nellore, Andhra Pradesh, India
Tel: +91-9440976666
E-mail: mandavabruno9@gmail.com
Received date: February 21, 2018; Accepted date: February 25, 2018; Published date: March 5, 2018
Citation: Unnam D, Singaraju GS, Mandava P, Reddy GV, Mallineni SK, et al. (2018) Accelerated Orthodontics– A review. J Dent Craniofac Res Vol.3 No.1:4. doi: 10.21767/2576-392X.100020
Abstract
Orthodontic treatment is the reorganization of skeletal and/or dental tissues. Prolonged treatment duration is one of the main concerns of patients undergoing with fixed orthodontics. This extended orthodontic treatment in such particular cases has several drawbacks to the patients such as increased predisposition to root resorption, dental caries and gingival recession, etc. Consequently, researchers introduced few methods to accelerate the velocity of the tooth movement without any drawbacks. These kind of methods used in orthodontics were popular as accelerated orthodontics. Accelerated orthodontics could be possible by mechanical stimulation or device assisted therapy, surgical therapy and by the use of pharmacological agents. The purpose of the present manuscript was to describe and evaluate the methods used in accelerated orthodontics.
Keywords
Accelerated orthodontics; Conventional orthodontic treatment; Corticotomy; Tooth movement
Introduction
The movement of tooth orthodontically happens under mechanical forces depends upon the alteration of the tissues surrounding its radicular part. These mechanical force creates a response in cellular component of surrounding periodontal ligament (PDL), that creates resorption in bone on pressure side and deposition of bone on the either side (tension side) [1]. This is an inflammatory process and the rate limiting factor for tooth movement is bone resorption at the bone and periodontal ligament interface [2]. Orthodontic movement can be controlled by the size of the applied force and the biological responses from the periodontal ligament [3]. This orthodontic force would cause around the periodontal ligament due to changes in blood flow, leading to the secretion of different inflammatory mediators like colony-stimulating factors, cytokines, growth factor, arachidonic acid metabolites and neurotransmitters. As a result of these secretions, remodelling of the bone occurs [4,5].
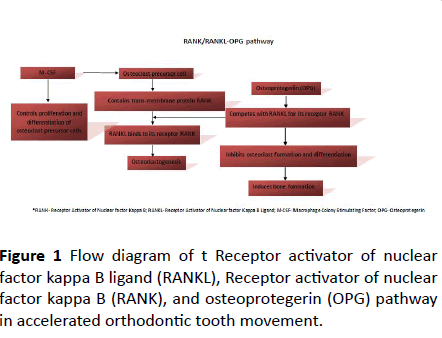
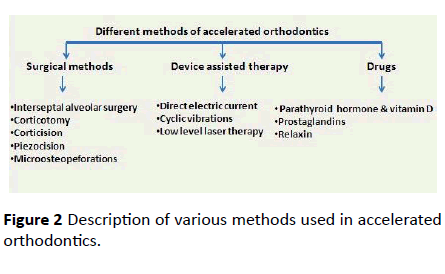
Macrophage colony stimulating factor (M-CSF), Receptor activator of nuclear factor kappa B ligand (RANKL), and osteoprotegerin (OPG) by osteoblasts play key roles in tooth movement has been showed in Figure 1. RANKL binds to its receptor, RANK (Receptor activator of nuclear factor kappa B), on the surface of osteoclastic cells at developmental stage. The RANKL/RANK binding is very critical for the function, differentiation, and survival of osteoclasts. Fixed orthodontics could last for 24 to 36 months which further poses the risk of complications associated with the treatment such as external root resorption, periodontal problems and patient compliance. Orthodontists are persistently motivated towards developing potential strategies to enhance the rate of orthodontic tooth movement [6-8]. The purpose of this article is to review and critically analyze the different methods of used for accelerating orthodontic tooth movement (AOTM) shown in Figure 2, indications, contraindications and their practical applications in clinical practice.
AOTM has been preferred for its numerous prospective benefits like shorter treatment duration, differential tooth movement, enhanced envelope of tooth movement, improved post treatment stability and reduced side effects [9]. Attempts to AOTM can be dated back to the 1890s, where Cunningham at a Chicago Dental Congress, described "luxation or immediate method in the treatment of irregular teeth". Cunningham [9] confined his treatment to palatally inclined maxillary lateral incisors with vertical inter-dental bone cuts and without the benefit of anesthesia. Subsequently there are various methods described in the literature on AOTM. The reported studies on accelerated orthodontics were analyzed based on evidence described by National Health and Medical Research Council [10].
Literature Review
Surgical methods
Direct injury to the both alveolar bones (maxillary arch and mandible arch) AOTM by inducing regional acceleratory phenomenon (RAP), as a wound-healing process, which is the basis for clinical procedures such as corticotomy-assisted orthodontics, piezocision-aided orthodontics, and surgery-first orthodontics [11,12]. Bichlmayr [5] introduced a surgical technique for hasty rectification of severe maxillary protrusion with available orthodontic appliances. Wedges of alveolar bone were removed to decrease the volume of the bone through the radicular parts of the maxillary teeth in anterior region. Kole [13] suggested a technique of creating bony blocks (bone-teeth unit) through the corticotomy to enhance the faster tooth movement. For the next fifty years this concept prevailed until Wilcko and co-workers [14], reported a transient demineralization -remineralization procedure enchanting after corticotomy, which was termed as a periodontally accelerated osteogenic orthodontics (PAOO). The PAOO is an amalgamation of selective decortications and facilitated orthodontic techniques along with alveolar augmentation. This procedure increases the alveolar bone volume after orthodontic treatment by using bone grafts consists of decalcified freeze-dried bone allograft (DFDBA). This technique decreases the treatment time to 33% the time of conventional treatment duration in orthodontics. This concept however was based on a similar technique, earlier described as Regional Acceleratory Phenomena (RAP) is local response to a lethal stimulus that describes a process of tissue formation faster than the usual local regeneration process. Enhancing a variety of healing stages, this RAP makes healing occur 2-10 times earlier than regular healing [15]. However, this is an old technique and very invasive hence, this was accepted by all patients. Hence, latest procedures like corticision, piezosurgery, fiberotomy and microosteoperforations had demonstrated (Table 1).
| Author | Technique | Type of study | Level of evidence | Type of study |
|---|---|---|---|---|
| Liou et al. [20] | Interseptal alveolar surgery | Cross sectional study | Level 3 | Human |
| Sukurica et al. [21] | Interseptal alveolar surgery | Cross sectional study | Level 3 | Human |
| Ren et al. [17] | Interseptal alveolar surgery | Randomised clinical trail | Level 2 | Animal |
| Leethanaku et al. [22] | Interseptal alveolar surgery | Randomised clinical trial | Level 2 | Human |
| Fischeret al. [25] | Corticotomy | Randomised clinical trail | Level 2 | Human |
| Lee et al. [26] | Corticotomy | Randomised clinical trail | Level 2 | Human |
| Mostaffa et al. [12] | Corticotomy | Randomised clinical trail | Level 2 | Animal |
| Aboul-ela et al. [27] | Corticotomy | Randomised clinical trail | Level 2 | Human |
| Shoreibah et al. [28] | Corticotomy | Randomised clinical trail | Level 2 | Human |
| Kim et al. [31] | Corticision | Cross sectional study | Level 3 | Animal |
| Jofre et al. [32] | Corticision | Case series | Level 4 | Human |
| Murphy et al. [33] | Corticision | Cross sectional study | Level 3 | Animal |
| Vercelotti et al. [35] | Piezocision | Case series | Level 4 | Human |
| Dibart et al. [36] | Piezocision | Case series | Level 4 | Human |
| Teixeria et al. [39], | MOP’s | Randomised clinical trail | Level 2 | Animal |
| Alikhani et al. [38] | MOP’s | Randomised clinical trail | Level 2 | Human |
Level 2- Randomised Clinical Trials. Level 3- Cross-Sectional, Case Control and Cohort Studies. Level 4- Case Series. MOP’S- Microosteoperforations.
Table 1: Studies performed using surgical methods.
Bone is surgically wounded so as to initiate a localized inflammatory response. The presence of cytokines and chemokines through prostaglandin E2 pathway and the RANK/ RANKL pathway causes differentiation of osteoclasts which leads to bone resorption and thus AOTM is possible. It has been reported that this effect lasts for 4 months the method needs to be repeated, in case faster tooth movement in further if required [16-39].
Inter-septal alveolar surgery: Inter-septal alveolar surgery or distraction osteogenesis involves controlled and gradual displacement of surgically created fractures which is termed as sub-periosteal osteotomy by incremental traction that results in simultaneous expansion of soft tissue and the bone volume due to mechanical stretching of the osteotomy site. It is divided into the distraction of the dentoalveolar bone or distraction of periodontal ligament [16].
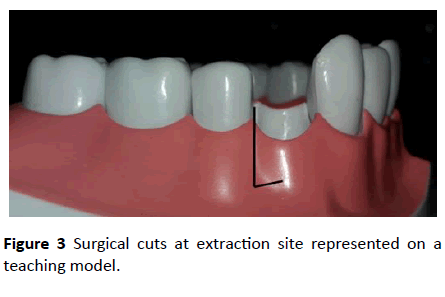
Procedure: At the time extraction of first premolars the inter-septal bone distal to the canine is undermined surgically. Eventually resistance on the pressure site will be reduced [17]. 1-1.5 mm in thickness distal to the canine undermined interseptally (Figure 3).
Distraction device used is a custom made, intraoral, toothborne device, manufactured from stainless steel [18].
Based on intersepatal alveolar surgery, the compact bone is replaced by the woven bone, and tooth movement is easier and quicker due to reduced resistance of the bone. It was found that these rapid movements are during the initial phases of tooth movement, especially in the first week [19]. In some cases rapid canine distraction of the dento-alveolar bone may be performed by the same principle of the distraction of periodontal ligament with the addition of more dissection and osteotomies performed at the vestibule. Several authors conducted human [20-22] and animal trails [17] (Table 2). By placing a custom-made distraction device and reported that alveolar surgery to be an effective and safe way to aid orthodontic tooth movement. Clinical trials on humans showed that periodontal distraction aided by surgical undermining of the inter-septal bone would reduce the resistance in the pathway of canine movement more effectively during orthodontic treatment. Among the studies reported on intr-septal alveolar surgery two were cross sectional studies and rest were randomized clinical trials (RCTs).
| Level | Design |
|---|---|
| I | Systematic review of Randomized controlled trials(RCTs) |
| II | Randomized controlled trials |
| III-1 | A pseudo-randomised controlled trial |
| III-2 | A comparative study with concurrent controls: Non randomised, experimental trial Case-control study Cohort study |
| III-3 | A comparative study without concurrent controls: Historical control study Two or more single arm study Interrupted time series without a parallel control group |
| IV | Case series with either a post-test or pre-test/post-test outcomes |
Table 2: Levels of evidence described by National Health and Medical Research Council (www.nhmrc.gov.au-2009).
Corticotomy: A corticotomy is defined as a surgical procedure whereby only the cortical bone is cut, perforated, or mechanically altered without any alteration in the medullary bone. This is performed without the involvement of medullary bone unlike osteotomies which involve the entire thickness of bone [24].
Procedure: Elevation of full thickness of buccala and/or lingual mucoperiosteal flaps. Positioning the corticotomy cuts using piezosurgical aurnameterium or micromotor under irrigation and it is followed by placement of a graft material, in required sites to enhance the thickness of the bone [24] (Figure 2).
Advantages: Bone can be augmented and periodontal defects would be avoided. Minimal changes in the periodontal attachment apparatus. Minimal treatment duration and increased rate of tooth movement. Less root resorption.
Disadvantages: Expensive and comparatively invasive procedure. May cause post-operative pain and swelling.
Various authors [12,25-28] performed clinical trials using corticotomy assisted canine retraction and found reduction in treatment time by 28%-33% and a 2-3-fold increase in velocity of tooth movement when compared with conventional OTM on control side. All the studies published on corticotomy were randomized clinical trials [12,25-28] among those one study [12] was animal study rest were involved with humans [25-28].
Corticision: Kim and co-workers [31] established a technique called corticision with minimal surgical intervention also called as minimally invasive rapid orthodontics (MIRO). Corticision was initiated as a supplemental dento-alveolar surgery in orthodontic therapy to achieve AOTM with minimal surgical intervention.
Procedure: Separation of the inter-proximal cortices with a reinforced scalpel is used as a thin chisel and a mallet transmucosally without reflecting a flap. With 45°-60° an inclination to the gingiva at the long axis of the canine a reinforced surgical blade with a minimum thickness of 400 μm should be located on the inter-radicular attachment. The surgical injury should be 2 mm from the papillary gingival margin in order to preserve the alveolar crest and should be 1 mm beyond the mucogingival junction. The blade should be pulled out by a swing motion. Clinical studies were conducted on humans [32] and animals [31,33] and concluded corticision effectively fastens tooth movement similar to corticotomy and is advantageous because of its less invasiveness. Among the published studies on cortision two were case control studies [31,33] and other was case series [31,32].
Piezocision: This is a minimally invasive procedure involves flapless in combining piezosurgical cortical micro-incisions with selective tunneling that allows for soft-tissue or bone grafting. [34] Vercelotti and Podesta [35] established the use of piezosurgery instead of burs, in conjunction with the conventional flap elevations to create an environment conducive for the rapid tooth movement. This technique is quite invasive as it requires extensive flap elevation and osseous surgeries, with post-surgical discomfort. This technique has not been widely accepted by patient community. Subsequently, Dibart [36] introduced piezocision with less invasiveness to this procedure.
Procedure: This is a combination of microincisions limited to the buccal gingiva that allows the use of a piezoelectric knife to give osseous cuts to the buccal cortex and initiate the RAP without involving palatal or lingual cortex [34]. The procedure allows for rapid tooth movement without the downside of an extensive and traumatic surgical approach while maintaining the clinical benefit of a soft-tissue or grafting concomitant with a tunnel approach. Only two human trials [35,36] were reported on the procedure
Dibart and co-workers [36,37] established a minimally invasive flapless procedure, combining micro incisions, piezoelectric incisions and selective tunneling that allows for hard- or soft-tissue grafting. They concluded that piezocision allows a rapid correction without the drawbacks of traumatic conventional corticotomy procedures in severe malocclusion cases. They later combined the technique with invisalign and it to be effective and esthetic.
Microosteoperforations (MOPs): A device called PropelTM, was launched by Propel Orthodontics to further reduce the invasive nature of surgical irritation of bone and this procedure was popularized as alveocentesis, which literally translates to puncturing bone [38]. The device has an adjustable depth dial adjustable at 0 mm, 3 mm, 5 mm, and 7 mm of tip depth and indicating arrow on the driver body. This device comes as ready-to-use sterile disposable device.
Procedure: A soft tissue flap was raised in the premolar and molar region and small perforations of about 0.25 mm are made using a round bur and hand piece through the cortical bone. Two RCTs were reported on microosteoperforations among these one was animal study [38] and other was human trial [39].
Contemporary status of surgical methods: Surgical methods are invasive procedures and patient cooperation is much needed. Inter-septal alveolar surgery, corticotomy and cortication are more invasive and expensive with needed surgical cuts and osteotomies. Post-operative complications are sometimes present with pain and swelling and patient discomfort. Recent techniques in surgical methods such as piezocision and microosteoperforations are less invasive with comparatively less complications, but more research should be done in using those techniques for accelerating the orthodontic tooth movement.
Device assisted therapy or mechanical stimulation methods: Direct electric currents, resonance vibration, low level laser therapy, static magnetic field, and pulsed electromagnetic field, were the methods used to accelerate tooth movement. The concept of using physical approaches came from the idea that applying orthodontic forces causes bone bending (bone bending theory) and bioelectrical potential develops. The bioelectrical potential is created when there is application of discontinuous forces, which leads to the idea of trying cyclic forces and vibrations (Table 3) [40-54].
| Author | Technique | Type of study | Level of evidence | Type of study |
|---|---|---|---|---|
| Zengo et al. [40] | Direct electric current | Case control study | Level 3 | Animal |
| Davidovitch et al. [41] | Direct electric current | Cross sectional study | Level 3 | Animal |
| Kim et al. [42] | Direct electric current | Randomised clinical trail | Level 2 | Human |
| Nishimura et al. [43] | Vibration | Cross sectional study | Level 3 | Animal |
| Liu et al. [44] | Vibration | Cross sectional study | Level 3 | Animal |
| Kau et al. [45] | Vibration | Randomised clinical trail | Level 2 | Human |
| Pavlin et al. [46] | Vibration | Randomised clinical trail | Level 2 | Human |
| Leethanakul et al. [47] | Vibration | Randomised clinical trail | Level 2 | Human |
| Kawasaki et al. [49] | LLLT | Cross sectional study | Level 3 | Animal |
| Cruz et al. [50] | LLLT | Randomised clinical trail | Level 2 | Human |
| Limpanichkul et al. [51] | LLLT | Randomised clinical trail | Level 2 | Human |
| Youssef et al. [52] | LLLT | Randomised clinical trail | Level 2 | Human |
| Doshi mehta et al. [53] | LLLT | Randomised clinical trail | Level 2 | Human |
| Genc et al. [54] | LLLT | Randomised clinical trail | Level 2 | Human |
Level 2- Randomised Clinical Trials. Level 3- Cross-Sectional, Case Control and Cohort Studies. LLLT- Low Level Laser Therapy
Table 3: Studies performed using mechanical stimulation.
Direct electric current: Electrical current has been tested experimentally on the animal models and have shown ATOM. Direct current or electrical currents generated piezoelectrically thereby enhance the AOTM.
Procedure: An electric appliance that provides direct electric current was placed in the extracted tooth region, generated bio electric potentials causing local responses and acceleration of bone modelling. This procedure was performed by some researchers [40,41] on living animals and found to be effective in tooth movement. Subsequently, Kim [42] performed a clinical trial on humans and found 30% acceleration of tooth movement when compared to conventional technique. Only three studies reported on this technique in the literature two were animal studies (one was case control study) [40] and cross section study [41] and one RCT [42] involved human trials.
Cyclic vibrations: The use of cyclic vibratory method is to place light alternating forces on the teeth via mechanical radiations. The initial response of cells to mechanical stress in vitro appears within 30 minutes.
Procedure: Signals from the force sensor and the accelerometer were transferred into the vibration controller. The amplified signal was then transferred to the vibrator, causing its excitation. The vibration was applied by the control signal through the power amplifier controlled by the output signal from the accelerometer, thereby maintaining the acceleration at 1.0 meter per square second (m/s2). A vibration-imposed system consists of a vibration controller, charge amplifier, vibrator, force sensor and accelerometer. The top of the vibrator was fixed on the tooth with an adhesive. The vibration tests were carried out for 5 minutes, and the resonance curves were displayed as frequency-force relationships on the monitor of the vibration controller. Clinical trials were conducted by various researchers [43-47] on human population using oral vibrating devices such as AccledentTM, AcceleDent® and electric tooth brushes and fund to be effective in increasing the rate of tooth movement. Two cross sectional animal studies [43,44] done on cyclic vibration.
Low-level laser therapy: Photo biomodulation or low-level laser therapy (LLLT) is one of the most promising approaches today. Laser light stimulates the proliferation of osteoclast, osteoblast and fibroblasts, and thereby affects bone remodeling and accelerates tooth movement. The mechanism involved in the acceleration of tooth movement is by the production of ATP and activation of cytochrome C [48] and improve the velocity of tooth movement via RANK/RANKL and the macrophage colony-stimulating factor and its receptor expression. Studies performed by numerous investigators [49-54] found LLLT has the potential to increase the rate of tooth movement. Limpanichkul [51] in their study did not found a significant result and concluded that the LLLT at the surface level in their study (25 J/cm2) was probably too low to express either stimulatory effect or inhibitory effect on the rate of orthodontic tooth movement. The variation amongst the studies seems to arise from variations in frequency of application of laser, intensity of laser, and method of force application on the tooth. Six studies performed on LLLT among those five were RCTs [50-54] done on humans and one study involve dcross sectional animal study [49].
Drugs: Parathyroid hormone, Vitamin D, Prostaglandins and Relaxin are the most commonly used pharmacological agents to increase the rate of tooth movement and thus decrease the treatment duration (Table 4) [55-66].
| Author | Year | Type of study | Level of evidence | Type of study |
|---|---|---|---|---|
| Soma et al. [55] | Parathyroid hormone | Case control study | Level 3 | Animal |
| Soma et al. [56] | Parathyroid hormone | Case control study | Level 3 | Animal |
| Collins et al. [57] | Vitamin D | Case control study | Level 3 | Animal |
| Kale et al. [58] | Vitamin D | Case control study | Level 3 | Animal |
| Kawakami et al. [59] | Vitamin D | Case control study | Level 3 | Animal |
| Yamasaki et al. [60] | Prostaglandins | Case control study | Level 3 | Animal |
| Yamasaki et al. [61] | Prostaglandins | Case control study | Level 3 | Animal |
| Yamasaki et al. [62] | Prostaglandins | Randomised clinical trail | Level 2 | Human |
| Selfi et al. [63] | Prostaglandins | Case control study | Level 3 | Animal |
| Liu et al. [64] | Relaxin | Case control study | Level 3 | Animal |
| Madan et al. [65] | Relaxin | Case control study | Level 3 | Animal |
| Mc Gorray et al. [66] | Relaxin | Randomised clinical trail | Level 2 | Human |
Table 4: Studies performed using drugs for accelerated orthodontics.
Parathyroid hormone: Calcium homeostatsis and bone remodeling in the human body are mainly regulated by parathyroid hormone (PTH). The main function of PTH is calcium reabsorption from small intestine and thus increases the serum calcium concentration. It causes absorption of calcium ions from bone and thus leads to bone resorption. This mechanism is taken advantage in accelerated orthodontics to fasten the tooth movement. Soma and coworkers [55,56] conducted experiments on rats and suggested that continuous administration of PTH is applicable to accelerate orthodontic tooth movement. Three animal case control studies [55-57] performed on parathyroid hormone used for AOTM.
Vitamin- D: Vitamin D has similar function as parathyroid hormone by calcium re-absorption. 1,25 dihydroxy vitamin D3, is the active form of vitamin D that act on small intestine causing calcium reabsorption. It has a similar action on bone and thus leads to bone resorption. Local administration of vitamin D in to PDL causes increase in LDH and CPK enzymes. Experimental studies were performed on rats by various investigators [57-59] and found 1, 25-DHCC to be more efficient in remodeling of bone during orthodontic tooth movement.
The studies so far performed where of short duration and the systemic effects of the hormone in long term such as kidney function and condition of long bones are not taken into consideration. Such disadvantages can be decreased by local administration using controlled release systems. Hence, a safe and effective release system is needed for better clinical use.
Prostaglandins: Prostaglandins (PGE) are paracrine lipid inflammatory mediators that act on nearby cells; PGE increase the number of osteoclasts directly which causes bone resorption. Primarily Yamasaki and co-workers [60,61] studied the effect of PGE in animal models by local administration and consequently, same group of researchers performed a clinical trial on humans and found that local administration of PGE, may cause safe and effective orthodontic tooth movement. Subsequently, Selfi and co-workers [63] investigated PGE2 in association with the calcium ions in controlling root resorption whereas significant increase in orthodontic tooth movement. Overall four studies were reported on PGE among those three were animal studies [60-62] and one was RCT [63].
Relaxin: Relaxin is a hormone which helps widening of the pubic ligaments in females during delivery; similarly, the presence of this hormone in cranial suture and PDL has been demonstrated. The role of relaxin is known for the remodeling of soft tissue rather than bone. Relaxin has the effect of increasing collagen at tension site and decreasing at pressure site. Experimental studies were performed on animal models [64,65] and the authors concluded that the human relaxin may not accelerate orthodontic tooth movement in rats; it can reduce the level of PDL, reduce the mechanical strength of PDL, and increase mobility of the tooth at early time points. Mc Gorray and co-workers [66] in their clinical trial found local doses of relaxin might have been too low to affect tooth movement or short-term relapse. Only three studies were available on the use relaxin are RCT [64,65] on humans and other two were case control studies done on animals [66].
Most of the pharmacological agents are restricted to the experimental studies because of their adverse effects either with systemic or local administration. Further studies are to be performed for their safe clinical use. But, all of these drugs have some or the other unwanted adverse effect. Hence, as of today, no drug exists that can safely accelerate orthodontic tooth movement.
Discussion and Conclusion
Acceleration of tooth movement while orthodontic treatment is of increasing demand now a day because of patient’s interest get the treatment completed in less span of time and to decrease the number of visits. Also, adult orthodontics has more demand as the number of adult patients is getting increased. Surgical techniques are more invasive and costly but are more beneficial with fewer side effects. Hence recent techniques such as piezocision, micro osteoperforations has the more demand in future. With increasing patient compliance, less invasive surgical techniques can be safely used to accelerate tooth movement. Device assisted therapy is also of high demand but there is a need for further studies about the proper device being used and how far it is useful. Pharmacological methods have more side effects and hence most of them are still in experimental stage. Only limited human trails are available. Accelerating orthodontic techniques can be highly useful for fastening the treatment as in every technique being used; there is increased rate of tooth movement and hence decreasing the treatment time.
References
- Davidovitch Z (1991) Tooth movement. Crit Rev Oral Biol Med 2: 411-50.
- Roberts WE, Huja S, Roberts JA (2004) Bone modeling: biomechanics, molecular mechanisms, and clinical perspectives. Semin Orthod 10: 123-161.
- Meikle MC (2008) The tissue, cellular, and molecular regulation of orthodontic tooth movement: 100 years after Carl Sandstedt. Eur J Orthod 28: 221-240.
- Davidovitch Z, Nicolay OF, Ngan PW, Shanfeld JL (1998) Neurotransmitters, cytokines, and the control of alveolar bone remodeling in orthodontics. Dent Clin North Am 32: 411-435.
- Bichlmayr A (1931) Chirurgische kieferothopaedie und das verhalten des knochens un der wurzelspitzen nach derselben. Deutsche Zahnaerztl Woschenschrift 34: 835-842.
- Theoleyre S, Wittrant Y, Tat SK, Fortun Y, Redini F, et al. (2004) The molecular triad OPG/RANK/RANKL: involvement in the orchestration of pathophysiological bone remodeling. Cytokine Growth Factor Rev 15: 457-475.
- Kaku M, Motokawa M, Tohma Y, Tsuka N, Koseki H, et al. (2008) VEGF and M-CSF levels in periodontal tissue during tooth movement. Biomed Res 29: 181-187.
- Maheshwari S, Verma SK, Tariq M, Gaur A (2015) Rapid orthodontics- A critical review. University J Dent Scie 1: 35-38.
- Hassan AH, Al-Fraidi AA, Al-Saeed SH (2010) Corticotomy-assisted orthodontic treatment: review. Open Dent J 4: 159-164.
- Levels of evidence described by National Health and Medical Research Council (www.nhmrc.gov.au-2009).
- Verna C, Dalstra M, Melsen B (2000) The rate and the type of orthodontic tooth movement is influenced by bone turnover in a rat model. Eur J Orthod 22: 343-352.
- Mostafa YA, Fayed MMS, Mehanni S, ElBokle NN, Heider AM (2009) Comparison of corticotomy-facilitated vs standard tooth movement techniques in dogs with miniscrews as anchor units. Am J Orthod Dentofacial Orthop 136: 570-577.
- Kole H (1959) Surgical operations on the alveolar ridge to correct occlusal abnormalities. Oral Surg Oral Med Oral Pathol 12: 515-529.
- Wilcko WM, Wilcko MT, Bouquot JE, Ferguson DJ (2001) Rapid orthodontics with alveolar reshaping: two case reports of decrowding. Int J Perio Resto Dent 21: 9-20.
- Frost HM (1983) The regional acceleratory phenomenon: a review. Henry Ford Hos Med J 31: 3.
- Mathews DP, Kokich VG (2013) Accelerating tooth movement: The case against corticotomy- induced orthodontics. Am J Orthod Dentofacial Orthop 144: 4-13.
- Ren A, Lv T, Kang N, Zhao B, Chen Y, et al. (2007) Rapid orthodontic tooth movement aided by alveolar surgery in beagles. Am J Orthod Dentofacial Orthop 131: 1-10.
- George JC, Thomas NO (2014) Distraction osteogenesis: Evolution and contemporary applications in orthodontics. J Res Pract Dent 2014: 1-20.
- Lv T, Kang N, Wang C, Han X, Chen Y, et al. (2009) Biologic response of rapid tooth movement with periodontal ligament distraction. Am J Orthod Dentofacial Orthop 136: 401-411.
- Liou EJW, Huang CS (1998) Rapid canine retraction through distraction of the periodontal ligament. Am J Orthod Dentofacial Orthop 114: 372-382.
- Sukurica Y, Karaman A, Gurel HG, Dolanmaz D (2007) Rapid canine distalization through segmental alveolar distraction osteogenesis. Angle Orthod 77: 226-236.
- Leethanakul C, Kanokkulchai S, Pongpanich S, Leepong N, Charoemratrote C (2014) Interseptal bone reduction on the rate of maxillary canine retraction. Angle Orthod 84: 839-845.
- Xue J, Ye N, Yang X, Wang S, Wang J, et al. (2014) Finite element analysis of rapid canine retraction through reducing resistance and distraction. J Appl Oral Sci 22: 52-60.
- Adusumilli S, Yalamanchi L, Yalamanchili PS (2014) Periodontally accelerated osteogenic orthodontics: An interdisciplinary approach for faster orthodontic therapy. J Pharm Bioallied Sci 1: 2-5.
- Fischer TJ (2007) Orthodontic treatment acceleration with corticotomy-assisted exposure of palatally impacted canines. Angle Orthod 77: 417-420.
- Lee JK, Chung KR, Baek SH (2007) Treatment outcomes of orthodontic treatment, corticotomy-assisted orthodontic treatment, and anterior segmental osteotomy for bimaxillary dentoalveolar protrusion (multicenter study, randomized controlled trial). Plast Reconstr Surg 120: 1027-36.
- Aboul-Ela SM, El-Beialy AR, El-Sayed KM, Selim EM, El-Mangoury NH, et al. (2011) Miniscrew implant-supported maxillary canine retraction with and without corticotomy facilitated orthodontics. Am J Orthod Dentofacial Orthop 139: 252-259.
- Shoreibah EA, Salama AE, Attia MS, Abu-Seida SM (2012) Corticotomy-facilitated orthodontics in adults using a further modified technique. J Int Acad Periodontol 14: 97-104.
- Long H, Pyakurel U, Wang Y, Liao L, Zhou Y, et al. (2013) Interventions for accelerating orthodontic toot movement: a systematic review. Angle Orthod 83: 164-171.
- Hassan AH, Al-Saeed SH, Al-Maghlouth BA, BahammamMA, Linjawi AI, et al. (2015) Corticotomy-assisted orthodontic treatment A systematic review of the biological basis and clinical effectiveness. Saudi Med J 36: 794-801.
- Kim J, Park YG, Kang SG (2009) Effects of corticision on paradental remodeling in orthodontic tooth movement. Angle Orthod 79: 284-291.
- Jofre J, Montenegro J, Arroyo R (2013) Rapid orthodontics with flapless piezoelectric corticotomies: First clinical experiences. Int J Odontostomat 7: 79-85.
- Murphy C, Kalajzic Z, Chandhoke T, Utreja A, Nanda R, et al. (2016) The effect of corticision on root resorption with heavy and light forces. Angle Orthod 86: 17-23.
- Dibart S, Sebaoun JD, Surmenian J (2009) Piezocision: a minimally invasive, periodontally accelerated orthodontic tooth movement procedure. Compend Contin Educ Dent 30: 342-50.
- Vercellotti T, Podesta A (2007) Orthodontic microsurgery: A new surgically guided technique for dental movement. Int J Periodontics Restorative Dent 27: 325-31.
- Dibart S, Sebaoun JM, Surmenian J (2011) Accelerated orthodontic treatments with Piezocision: a mini–invasive alternative to alveolar corticotomies. Orthod Fr 82: 311-319.
- Keser EI, Dibart S (2011) Piezocision-assisted Invisalign treatment. Compend Contin Educ Dent 32: 46-8; 50-1.
- Alikhani M, Raptis M, Zoldan B, Sangsuwon C, Lee YB, et al. (2013) Effect of micro-osteoperforations on the rate of tooth movement. Am J Orthod Dentofacial Orthop 144: 639-648.
- Teixeira CC, Khoo E, Tran J, Chartres I, Liu Y, et al. (2010) Cytokine expression and accelerated tooth movement. J Dent Res 89: 1135-1141.
- Zengo AN, Bassett CA, Pawluk RJ, Prountzos G (1974) In vivo bioelectric potentials in the dentoalveolar complex. Am J Orthod 66: 130-139.
- Davidovitch Z, Finkelson MD, Steigman S, Shanfeld JL, Montgomery PC, et al. (1980) Electric currents, bone remodeling, and orthodontic tooth movement. II. Increase in rate of tooth movement and periodontal cyclic nucleotide levels by combined force and electric current. Am J Orthod 77: 33-47.
- Kim DH, Park YG, Kang SG (2008)The effects of electrical current from a micro-electrical device on tooth movement. Korean J Orthod 38: 337-346.
- Nishimura M, Chiba M, Ohashi T, Sato M, Shimizu Y, et al. (2008) Periodontal tissue activation by vibration: intermittent stimulation by resonance vibration accelerates experimental tooth movement in rats. Am J Orthod Dentofacial Orthop 133: 572-583.
- Liu D (2010) Acceleration of orthodontic tooth movement by mechanical vibration. AADR Annual meeting Washington D.C.
- Kau CH, Jennifer TN, Jeryl D (2010) The clinical evaluation of a novel cyclical-force generating device in orthodontics. Orthodontic Practice US 1: 43-44.
- Pavlin D, Anthony R, Raj V, Gakunga PT (2015) Cyclic loading (vibration) accelerates tooth movement in orthodontic patients: A double-blind, randomized controlled trial. Sem Orthod 21: 187-94.
- Leethanakul C, Suamphan S, Jitpukdeebodintra S, Thongudomporn U, Charoemratrote C (2016) Vibratory stimulation increases interleukin-1 beta secretion during orthodontic tooth movement. Angle Orthod 86: 74-80.
- Fujita S, Yamaguchi M, Utsunomiya T, Yamamoto H, Kasai K (2008) Low-energy laser stimulates tooth movement velocity via expression of RANK and RANKL. Orthod Craniofac Res 11: 143-55.
- Kawasaki K, Shimizu N (2000) Effects of low-energy laser irradiation on bone remodeling during experimental tooth movement in rats. Lasers Surg Med 26: 282-291.
- Cruz DR, Kohara EK, Ribeiro MS, Wetter NU (2004) Effects of low-intensity laser therapy on the orthodontic movement velocity of human teeth: A preliminary study. Lasers Surg Med 35: 117-120.
- Limpanichkul W, Godfrey K, Srisuk N, Rattanayatikul C (2006) Effects of low-level laser therapy on the rate of orthodontic tooth movement. Orthod Craniofac Res 9: 38-43.
- Youssef M, Ashkar S, Hamade E, Gutknecht N, Lampert F, et al. (2008) The effect of low-level laser therapy during orthodontic movement: a preliminary study. Lasers Med Sci 23: 27-33.
- Doshi Mehta G, Bhad Patil WA (2012) Efficacy of low-intensity laser therapy in reducing treatment time and orthodontic pain: a clinical investigation. Am J Orthod Dentofacial Orthop 141: 289-297.
- Genc G, Kocadereli I, Tasar F, Kilinc K, El S, et al. (2013) Effect of low-level laser therapy (LLLT) on orthodontic tooth movement. Lasers Med Sci 28: 41-47.
- Soma S, Iwamoto M, Higuchi Y, Kurisu K (1999) Effects of continuous infusion of PTH on experimental tooth movement in rats. J Bone Miner Res 14: 546-554.
- Soma S, Matsumoto S, Higuchi Y, Takano-Yamamoto T, Yamashita K, et al. (2000) Local and chronic application of PTH accelerates tooth movement in rats. J Dent Res 79: 1717-1724.
- Collins MK, Sinclair PM (1988) The local use of vitamin D to increase the rate of orthodontic tooth movement. Am J Orthod Dentofacial Orthop 94: 278-284.
- Kale S, Kocadereli I, Atilla P, As E (2004) Comparison of the effects of 1,25 dihydroxycholecalciferol and prostaglandin E2 on orthodontic tooth movement. Am J Orthod Dentofacial Orthop 125: 607-614.
- Kawakami M, Takano-Yamamoto T (2004) Local injection of 1,25-dihydroxyvitamin D3 enhanced bone formation for tooth stabilization after experimental tooth movement in rats. J Bone Miner Metab 22: 541-546.
- Yamasaki K, Miura F, Suda T (1980) Prostaglandin as a mediator of bone resorption induced by experimental tooth movement in rats. J Dent Res 59: 1635-1642.
- Yamasaki K, Shibata Y, Fukuhara T (1982) The effect of prostaglandins on experimental tooth movement in monkeys (Macaca fuscata). J Dent Res 61: 1444-1446.
- Yamasaki K, Shibata Y, Imai S, Tani Y, Shibasaki Y, et al. (1984) Clinical application of prostaglandin E1 (PGE1) upon orthodontic tooth movement. Am J Orthod 85: 508-518.
- Seifi M, Eslami B, Saffar AS (2003) The effect of prostaglandin E2 and calcium gluconate on orthodontic tooth movement and root resorption in rats. Eur J Orthod 25: 199-204.
- Liu ZJ, King GJ, Gu GM, Shin JY, Stewart DR (2005) Does human relaxin accelerate orthodontic tooth movement in rats? Ann N Y Acad Sci 1041: 388-394.
- Madan MS, Liu ZJ, Gu GM, King GJ (2007) Effects of human relaxin on orthodontic tooth movement and periodontal ligaments in rats. Am J Orthod Dentofacial Orthop 131: 1-10.
- McGorray SP, Dolce C, Kramer S, Stewart D, Wheeler TT (2012) A randomized, placebo-controlled clinical trial on the effects of recombinant human relaxin on tooth movement and short-term stability. Am J Orthod Dentofacial Orthop 141: 196-203.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences