Abusive Maternal Care and Associated factors during Childbirth in Ethiopia during COVID-19 Pandemic
Lebeza Alemu* and Melese Linger Endalifer
Department of Midwifery, College of Health Sciences, Woldia University, Woldia, Ethiopia
- *Corresponding Author:
- Lebeza Alemu
Department of Midwifery, College of Health Sciences
Woldia University, Woldia, Ethiopia
E-mail: lebezaa@gmail.com
Received Date: December 29, 2020; Accepted Date: January 12, 2021; Published Date: January 19, 2021
Citation: Alemu L, Endalifer ML (2020) Abusive Maternal Care and Associated Factors during Childbirth in Ethiopia during COVID-19 Pandemic. J Women’s Health Reprod Med Vol. 5 No.1:1.
Abstract
Skilled birth attendance during childbirth and immediate postpartum care can prevent 75% of maternal mortality. This is an emerging global pandemic infectious caused by a newly discovered coronavirus since December 2019 called COVID-19 which affects the health service care including maternal health care services. The care given in the health institution is not psychologically supportive of what they need. Therefore, this study aimed to assess the level of abusive maternal care and associated factors during childbirth in Ethiopia during the global pandemic disease (COVID-19). The institutional-based cross-sectional study design was implemented in 2020 with a sample size of 394. Data was collected by using a structured questionnaire adapted from the White Ribbon Alliance Declaration of women's right during childbirth. The data were used logistic regression analysis method. The level of abusive care among childbearing women was 47.1%. Women who attended their childbirth at the general hospital, women who had no antenatal care and women who had two birth attendants were significantly associated with abusive maternal care.
Keywords
Abusive maternal care; Associated factors; Women; Ethiopia
Abbreviations
ANC: Antenatal Care; AOR: Adjusted Odds Ratio; CI: Confidence Interval; FIGO: Federation of international Gynaecology and obstetrics; SPSS: Statistical Package for the Social Sciences; WHO: World Health Organization
Introduction
On 9 January 2020, the World Health Organization (WHO) officially announced the discovery of a novel coronavirus, SARSCov2 which is recognized as highly pathogenic viral strains responsible for infectious respiratory disease (COVID-19) which affect including the health care system [1].
In the globe, around 303,000 women die annually of these 201,000 deaths were from Sub-Saharan Africa [2]. In Ethiopia, maternal mortality and morbidity levels are among the highest in the world which was 412 per 1, 00,000 live births in 2016 [3].
Even though skilled birth attendance during childbirth and immediate postpartum care can prevent 75% of maternal mortality only 26% of women deliver their baby at health institutions [4].
Abusive care is a comprehensive term that is expressed in the form of physical abuse, non-consented care, non-confidential care, non-dignified care, discrimination based on specific patient attributes, abandonment of care, and detention in facilities [5].
This respectful maternity care is a universal right of every woman which is chartered at different times and compiled by in White ribbon alliance in 2011 [6].
Enhancing institutional delivery coverage is a primary action to tackle maternal mortality, but abusive maternal care during childbirth decreases women’s intention on institutional delivery [5]. Skilled birth attendance during childbirth and immediate postpartum care can prevent 75% of maternal mortality but women are not willing to deliver in the health institutions due to ignorance of their sensitive issues by health professionals and the care given in the health institution is not psychological supportive of what they need [4,7].
Most countries affected by the pandemic were able to slow down the spread of the coronavirus with varying degrees of success, like banning public events and gatherings, workplace closures, stayat- home restrictions, restrictions on domestic and international transport, and shutting some health care services [8].
In South Africa, women are not volunteers to attend their pregnancy follow up at the health institution because midwives were so rude and would only go when in labour [9]. Nigerian women also do not utilize maternal health care at health institutions due to prior uncomfortable health service experiences or the fear of being humiliated by the health care Staff [10].
A study conducted in Kenya revealed that the prevalence of any abusive care facing the women during service utilization was 20% [11] which was 78.6% at governmental health institutions Addis Ababa Ethiopia [12].
Although abusive care during childbirth is not only threatened their rights to life, health, bodily integrity, freedom from discrimination but also deny institutional delivery preference of the women. Therefore, this study aimed to assess the level of abusive maternal care and associated factors during childbirth in North Wollo Hospitals, Northeast Ethiopia.
Methods
Study settings
An institution-based cross-sectional study was conducted in North Wollo governmental hospitals from June 20 to August 30, 2020. Even though there were five governmental hospitals in North Wollo, Ethiopia, two hospitals were taken as a study institution. The study was conducted at Woldia general hospital and Lalibela primary hospital. The study population was women who gave birth in selected hospitals in the study period. Women with postpartum psychiatric problems and women who referred for complication management after they gave birth in the other health institution were excluded.
Sample size determination and sampling procedure
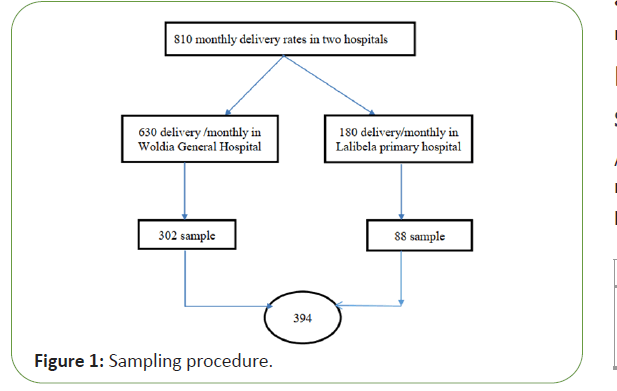
The sample size was determined by using a single population proportion formula with the following assumptions, Proportion of abusive care in Addis Ababa governmental hospital was 81.8% [12], marginal error (4%), and considering 10% for non-response rate. Therefore the final sample size was 394.
Sampling procedure
A stratified systematic random sampling technique was applied. The sample was proportionally allocated to the hospitals based on the patient flow rate of the delivery ward in one month period before the actual data collection period (Figure 1).
Operational definitions
Abusive maternal care: if the score of abusive maternal care assessing questions is greater than the mean score (21.12) the study considered the mother faced abusive care.
Data collection tools and procedure
Data were collected from women who gave birth in respective hospitals immediately at the time of discharge through the exit interview. The questionnaire has three parts, the first sociodemographic characteristics, obstetric history, and abusive maternal care assessing parts (seven performance indicators and thirty-one verification criteria). To assess women’s abusive care during childbirth the questionnaire was adopted from White Ribbon Alliance, Federation of international gynaecology and obstetrics and Maternal and Child Health Integrated Program standards of respectful maternity care tool kit. The organization listed above has prepared using seven performance standards and their respective verification criteria.
The seven performance standards are physical abuse, nonconsented care, non-confidential care, non-dignified care (including verbal abuse), discrimination based on specific attributes, abandonment or denial of care, and detention in facilities [13]. Six female data collectors who are not working in the respective hospitals were recruited to collect the data.
Data quality assurance
The questionnaire was prepared in English first then it was translated to the Amharic language by language professionals and translated back to English to maintain consistency. A pretest was conducted at Woldia health center before two weeks of actual data collection period in 5% of the sample size. The data collector was given training and supervision were done daily to check the completeness of the questionnaire and to evaluate daily activities.
Data processing and analyses
The data were checked for completeness after data collection and entered into Epi Data version 3.1 and analysed by using SPSS version 23. Descriptive statistics were used to present the data. The question has a binary response (yes/no). "Yes" scored as "1" and "No" is scored as "0". Bivariate and multivariable logistic regression analysis was carried out. Model fitness was assured.
Results
Socio-demographic characteristics
A total of 382 respondents were interviewed with a non-response rate of 3% (12 discontinued the survey). The majority of study participants were in the age range of 20-34 years (Table 1).
| Characteristics | Categories | Frequency (%) |
|---|---|---|
| Age | <20 | 7(1.8) |
| 20-34 | 332(86.4) | |
| 35-49 | 43(11.1) | |
| Marital status | Married | 336(87.5) |
| Unmarried | 32(8.3) | |
| Divorced | 9(2.3) | |
| Other | 5(1.3) | |
| Educational status | No education | 122(31.7) |
| Elementary | 122(31.7) | |
| Secondary | 86(22.3) | |
| College and above | 51(13.2) | |
| Occupational status | Housewife | 200(52.3) |
| Merchant | 69(18) | |
| Unemployed | 30(7.8) | |
| Employed | 46(12) | |
| Daily laborer | 18(4.7) | |
| Farmer | 10(2.6) | |
| Other | 10(2.6) | |
| Residence | Urban | 238(62.3) |
| Rural | 144(37.7) |
Table 1: Socio-demographic characteristics of childbearing women in Northeast Ethiopia, 2020(n=382).
Obstetric characteristics
Regarding the previous history of institutional delivery, only 50% of them were delivered at the health institution 200 (52%) of women attending ANC in their previous pregnancy (Table 2).
| Characteristics | Categories | Frequency (%) |
|---|---|---|
| Gravidity | 1 | 139(36.3) |
| 02-Mar | 195(51.1) | |
| >=4 | 48(12.6) | |
| The previous history of ANC follow up | Yes | 200(52) |
| No | 172(44.7) | |
| Previous institutional delivery history | Yes | 191(50) |
| No | 191(50) | |
| Duration after delivery | 0-6 | 111(58.1) |
| 6-24 hrs | 50(26.2) | |
| >24 hrs | 30(15.7) | |
| Number of birth attendant | One | 28(14.6) |
| Two | 95(49.7) | |
| >=3 | 68(35.6) | |
| Sex of birth Attendant | Male | 60(31.4) |
| Female | 35(18.3) | |
| Both sex | 96(50.3) | |
| Type of hospital | Primary | 80(20.9) |
| General | 302(79.1) | |
| Access other than a health care provider | Yes | 33(17.3) |
| No | 158 (82.7) | |
| Have you get any birth-related complication | Yes | 103(27) |
| No | 279(73) |
Table 2: Obstetric characteristics of childbearing women in Northeast Ethiopia, 2020(n=382).
Level of abusive maternal care among childbearing women
The assessment of abusive maternal care was addressed through the white ribbon alliance declaration rights of childbearing women. This white ribbon alliance declaration has seven performance indicators. Generally, all most all mothers (99.2%) were suffered from at least one abusive care from thirty-one verification criteria. By using mean as cut off point the level of abusive care among childbearing women was 47.1%.
About 97.3% of women were suffered from at least one physical abuse component. A woman abused from physical force (slapping, aggressiveness, and beating) was 90.8%. Respect for women receiving care according to culture 90.1% was not treated accordingly. The prevalence of non-consented care was 98.6% (that means they receive a minimum of one no consented care from the components). From all participants, 65.2%were greeted by the health care provider, and only 27.7% were introduced by the health care provider. Of the total study participants, 96.6% of women receive non-confidential care. Of the total 86.1% of the client’s information was protected from being transferred to others. Only 49.5% were gain drape to cover the lower part of the abdomen during diagnosis by the health care provider.
The overall prevalence of non-dignified care was 99% (that means they receive a minimum of one non-dignified care). From the total participants, only 18% of women were encouraged to practice cultural activities like (praying, reading spiritual books, and holly pictures). Of the total women, 98.7% of women were discriminated during childbirth. Among the total 96.6% of health care providers were communicating to the women in a language that she understands. An additional 84.6% of health care providers didn't show any disrespect to what she responds. The prevalence of abandonment of care during childbirth was 97.4%. Almost all mothers receive essential basic care for women. Around 80% of women were well informed by a health care provider to call when they want and 86.4% of women were not left alone in the delivery room. The overall prevalence of detained care during childbirth in hospitals was 4.5%. More than 97% were not detaining against their will and due to a lack of payment (Table 3).
| Abusive care (n=382) | |||
|---|---|---|---|
| Performance indicator | Verification criteria | Yes (%) | No (%) |
| Any form of physical abuse | 372(97.4) | 10(2.6) | |
| Uses physical force or abrasive behavior | 347(90.8) | 35(9.2) | |
| treated according to their culture | 38(9.9) | 344(90.1) | |
| Abandoning of body movement during labour | 13(3.4) | 369(96.6) | |
| Have you denied to drink and to eat food during labour | 95(24.9) | 287(75.1) | |
| Get pain relief activity | 75(19.6) | 307(80.4) | |
| The unnecessary separation between child and mother | 344(90.1) | 38(9.9) | |
| Any form of non-consented care | 377(98.6) | 5(1.3) | |
| Get greeting from the health care provider | 249(65.2) | 133(34.8) | |
| Introduces self to a woman and her companion | 106(27.7) | 276(72.3) | |
| Encourages companion to remain with a woman whenever possible | 321(84) | 61(16) | |
| Encourages woman and her companion to ask questions | 202(52.9) | 180(47.1) | |
| Responds to questions with promptness, politeness, and truthfulness | 269(70.4) | 113(29.6) | |
| Explains what is being done and Gives information on the status and findings of an examination | 340(89) | 42(11) | |
| Obtains consent or permission before any procedure | 344(90) | 38(10) | |
| Denying choice of position for birth | 223(58.4) | 159(41.6) | |
| Denying liberty of movement during labor | 313 (82) | 69(18) | |
| Get information on the progress of labor | 344(90) | 38(10) | |
| Any form of non-confidential care | 369(96.6) | 13(3.4) | |
| Shared client information with others without permission | 53(13.9) | 329(86.1) | |
| Uses curtains or other visual barriers to protect a woman during exams, procedures | 270(70.7) | 112(29.3) | |
| Uses drapes or covering appropriate to protect woman’s privacy | 189(49.5) | 193(50.5) | |
| leave client records in area where they can be read by others not involved in the care | 46(12) | 336(88) | |
| Any form of non-dignified care | 378(99) | 4(1) | |
| Speaks politely to woman and companion | 357(93.5) | 25(6.5) | |
| Insults, intimidation, threats, or coerces woman or her companion | 46(12) | 336(88) | |
| Encouraged to practice cultural activities during labour like praying | 69(18) | 313(82) | |
| Any form of discriminated care | 377(98.7) | 5(1.3) | |
| Speaks to the woman in a language and at a language level that she understands | 369(96.6) | 13(3.7) | |
| show disrespect to women based on any specific attribute/response | 59(15.4) | 323(84.6) | |
| Any form of abandonment of care | 372(97.4) | 10(2.6) | |
| Provides basic essential care to the woman | 373(97.6) | 9(2.4) | |
| Get informed to call health care provider while she wants | 306(80) | 76(29) | |
| health care provider comes immediately while she wants | 342(89.5) | 40(10.5) | |
| Left alone at the delivery room | 330(86.4) | 52(13.6) | |
| Any form of details | 17(4.5) | 365(95.5) | |
| Detains a woman against her will | 8(2) | 374(98) | |
| Detention of the woman in the facility due to lack of payment of facility fees | 11(2.9) | 371(97.1) | |
Table 3: Level abusive maternal care childbearing women Northeast Ethiopia, 2020 (n=382).
Factors associated with abusive care
In multivariable logistic regression analyses women who attend their childbirth at a general hospital, women who have antenatal care, and the number of birth attendants were significant association with abusive maternal care.
Women who attended their childbirth at general hospital 87% (AOR=0.13, 95% CI: 0.06, 0.26) decreases the odds of abusive maternal care as compared to the primary hospital. Women who had no antenatal care 2.08 times (AOR=2.08, 95% CI: 1.27, 3.39) higher the odds of abusive maternal care as compared to have ANC follow up.
Women attended by one health care provider (AOR=0.29, 95% CI: 0.1, 0.84) decreases the likelihood of abusive maternal care by 71% as compared to a woman attended by more than three health care providers. Receiving abusive maternal care among women attended by two health care providers lowered by 44% as compared to a woman attended by more than three health care providers (AOR=0.56, 95% CI: 0.35,0.92) (Table 4).
| Abusive care | |||||
|---|---|---|---|---|---|
| Variables | Yes | No | AOR (95%CI) | P-value | |
| Type of hospital | General | 112 | 190 | 0.131(0.066-0.261) | 0.0001 |
| Primary | 68 | 12 | 1 | ||
| Residence | Rural | 71 | 73 | 1.671(0.984-2.838) | 0.058 |
| Urban | 109 | 129 | 1 | ||
| History of ANC follow up | No | 102 | 70 | 2.080(1.277-3.390) | 0.003 |
| Yes | 78 | 132 | 1 | ||
| Occupational status | Housewife | 72 | 128 | 0.440(0.129-1.495) | 0.188 |
| Merchant | 29 | 40 | 0.716(0.198-2.590) | 0.61 | |
| Unemployed | 21 | 9 | 0.902(0.212-3.842) | 0.889 | |
| Employed | 31 | 15 | 1.510(0.392-5.808) | 0.549 | |
| Daily labourer | 13 | 5 | 1.5150.301-7.631() | 0.614 | |
| Farmer | 14 | 5 | 1 | ||
| Number of birth attendant | one birth attendant | 7 | 21 | 0.29(0.1-0.845) | 0.023 |
| 2 birth attendant | 87 | 106 | 0.568(0.35-0.923) | 0.023 | |
| >2 birth attendant | 86 | 75 | 1 | ||
Table 4: Multivariable regression table factor associated with abusive care during childbirth Northeast Ethiopia, 2020(n=382) Hosmer Lemeshow: P-value=0.742 1 =reference category Backward LR method was applied.
Discussion
The level of abusive care in this study was 47.1% (95% CI 42.1- 52.6). This finding is similar to a systemic review done on the mistreatment of women during childbirth in health facilities globally [14]. The finding of this study is lower than the study done in Addis Ababa which might be due to the study was implemented from the health care providers unlike this study [15].
Among the study participants, about 97.4% of women were suffered from at least one physically abuse(physical force or abrasive behaviour, not treated according to her culture, abandoning of body movement during labour, denied to drink and to eat food during labour, didn't get pain relief activity and unnecessary separation between child and mother) which is higher than research conducted in Addis Ababa with a prevalence of physical abuse 2.3% [16] and 35.7% in Kenya [17]. This difference may result from socio-demographic variations among study participants.
Another study conducted in six countries of Africa (Ethiopia, Kenya, Zanzibar, Rwanda, Madagascar, and Tanzania) through observation technique to assess abusive maternity care; the observer report applying episiotomy for all prime-gravida women were a routine practice in Ethiopia health facility which harm women's physically but this is not a common problem in the current study [18].
Regarding non-consented care, 98.6% have received a minimum of one no consented care this is supported by other researchers [19,20]. This figure is much greater than the study conducted in Tanzania [21]. From the components 41.3% of women were denied position preference during childbirth; this figure is much higher than a study conducted in Addis Ababa with a proportion of 29% [22]. The variation might be the current study apply exit interview the latter one conducted through direct observation; collecting data by direct observation gives more reliable data.
From all study participants 96.6%, 99%, 98.7%, 99.4% of women receive non-confidential, discriminated, and abandonment care respectively. This is also mentioned in other studies conducted elsewhere [22-25,20,17]. Confidentiality is mandatory and if it is not corrected early, it leads to a crisis in health care delivery.
From the total participants, only 18% of women were encouraged to practice cultural activities like (praying, reading spiritual books and holly picture), which shows there is a restriction on women to express their feelings in the health institution this may result in spiritual stress, loneliness and complicate the outcome of labour. This is strongly evidenced by the obstetric care navigation approach: disrespectful care was highly experienced when cultural and contextual differences between indigenous patients and non-indigenous providers present [26].
The overall prevalence of detained care during childbirth in hospitals was 4.5%, this is lower than a study conducted in Nigeria [17], In other study conducted in Addis Ababa reported that women's are free of detention care [20]. This is due to the declaration of giving payment free service in the maternity ward by the Ethiopian government health policy.
Women who attend their childbirth at general hospitals decrease the occurrence of abusive maternal care as compared to a primary hospital which may be due to the standard difference among hospitals and the number of health professionals with many speciality may available in the general hospitals than primary hospitals.
Women who had no ANC follow up previously increase the occurrence of abusive maternal care as compared to those who had previous ANC follow-ups. Mothers who have ANC follow up may develop friendly relationship with the health care providers which make their delivery time easy and respectful.
Women attended her delivery by one or two health care providers’ decreases the likelihood of abusive maternal care as compared to a woman attended by more than three health care providers. The possible reason may be as the number of birth attendants increases the client's privacy, information, confidentiality will have no guarantee, and this increases the occurrence of abusive maternal care during childbirth.
Social desirability bias is one of the limitations of this study since women may report more acceptable response. The questionnaire also does not address misleading medical procedures (aseptic technique, medical error, maleficence). This study did not establish cause and effect relationship between independent and outcome variable due to the limitation of cross-sectional study design.
Conclusion
The level of abusive maternal care in the health institutions was high as compared to different international declarations which affect women’s willingness to attend their childbirth in the health facility which is directly related with the impact of CVID- 19. Women who attend their childbirth at general hospitals, having antenatal care visits, and the number of birth attendants were significantly associated with abusive maternal care. The interventions better to focus on increasing pregnant women’s ANC follow up. Health institutions also better increase the number of skilled birth attendants to address women’s concerns during childbirth.
Declarations
Ethical considerations
Ethical clearance was obtained from Woldia University ethical clearance committee. A formal letter was given to the selected health institutions from the school of public health. Moreover, informed verbal consent was obtained from each respondent since our study participants are not literate and they informed their right to withdraw from the study at any time. Confidentiality and privacy of participants were secured by omitting any identifier.
Consent for publication
Not applicable.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Competing interest
The authors declare that they have no competing interests.
References
- Marinoni G, Vant Land H, Jensen T (2020) The impact of Covid-19 on higher education around the world. IAU Global Survey Report.
- Alkema L, Chou D, Hogan D, Zhang S, Moller AB, et al. (2016) Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Maternal Mortality Estimation Inter-Agency Group. Lancet 387: 462-474.
- Survey DaH (2011) Maternal and perinatal country profile. Ethiopia: Department of Maternal, Newborn, Child and Adolescent Health.
- Central Statistical Agency (CSA) (2016) [Ethiopia] and ICF. Ethiopia Demographic and Health Survey. Addis Ababa, Ethiopia, and Rockville, Maryland, USA: CSA and ICF.
- Bowser D, Hill K (2010) Exploring evidence for disrespect and abuse in facility-based childbirth. Boston: USAID-TRAction Project. Harvard T.H. Chan School of Public Health.
- Alliance WR (2011) Respectful maternity care: the universal rights of childbearing women. WRA.
- Shiferaw S, Spigt M, Godefrooij M, Melkamu Y, Tekie M (2013) Why do women prefer home births in Ethiopia?. BMC Pregnancy Childbirth 13: 5.
- Edelson DP, Sasson C, Chan PS, Atkins DL, Aziz K, et al. (2020) Interim guidance for basic and advanced life support in adults, children, and neonates with suspected or confirmed COVID-19: From the emergency cardiovascular care committee and get with the guidelines®-Resuscitation adult and pediatric task forces of the American Heart Association in Collaboration with the American Academy of Pediatrics, American Association for Respiratory Care, American College of Emergency Physicians, The Society of Critical Care Anesthesiologists, and American Society of Circulation.
- Jewkes R, Abrahams N, Mvo Z (1998) Why do nurses abuse patients? Reflections from South African obstetric services. Soc Sci Med 47: 1781-1795.
- Centre for Reproductive Rights and Women Advocates Research and Documentation Centre. Broken promises: human rights, accountability, and maternal death in Nigeria.
- Abuya T, Warren CE, Miller N, Njuki R, Ndwiga C, et al. (2015) Maranga A, Mbehero F, Njeru A, Bellows B. Exploring the prevalence of disrespect and abuse during childbirth in Kenya. PloS one 10: e0123606.
- Asefa A, Bekele D (2015) Status of respectful and non-abusive care during facility-based childbirth in a hospital and health centers in Addis Ababa, Ethiopia. Reprod Health 12: 33.
- Stein CA (2019) Respectful Maternity Care in Santa Cruz County, California (Doctoral dissertation, University of Hawai'i at Manoa).
- Bohren MA, Vogel JP, Hunter EC, Lutsiv O, Makh SK, et al. (2015) The mistreatment of women during childbirth in health facilities globally: a mixed-methods systematic review. PLoS Med 12: e1001847.
- Sacks E (2017) Defining disrespect and abuse of newborns: a review of the evidence and an expanded typology of respectful maternity care. Reprod Health 14: 66.
- Asefa A, Bekele D (2015) Status of respectful and non-abusive care during facility-based childbirth in a hospital and health centers in Addis Ababa, Ethiopia. Reprod Health 12: 33.
- Okafor II, Ugwu EO, Obi SN (2015) Disrespect and abuse during facility-based childbirth in a low-income country. Int J Gynecol 128: 110-113.
- Rosen HE, Lynam PF, Carr C, Reis V, Ricca J, et al. (2015) Direct observation of respectful maternity care in five countries: a cross-sectional study of health facilities in East and Southern Africa. BMC Pregnancy Childbirth 15: 306.
- Sando D, Abuya T, Asefa A, Banks KP, Freedman LP, et al. (2017) Methods used in prevalence studies of disrespect and abuse during facility based childbirth: lessons learned. Reprod Health 14: 1-8.
- Daniel E. Identifying and Measuring Women’s Perception of Respectful Maternity Care in Public Health Facilities. Institute of Psychology. ADDIS ABABA.
- Sando D, Ratcliffe H, McDonald K, Spiegelman D, Lyatuu G, et al. (2016) The prevalence of disrespect and abuse during facility-based childbirth in urban Tanzania. BMC Pregnancy Childbirth 16: 236.
- Sheferaw ED, Bazant E, Gibson H, Fenta HB, Ayalew F, et al. (2017) Respectful maternity care in Ethiopian public health facilities. Reprod Health 14: 60.
- Savage V, Castro A (2017) Measuring mistreatment of women during childbirth: a review of terminology and methodological approaches. Reprod Health 14: 138.
- Asefa A, Bekele D, Morgan A, Kermode M (2018) Service providers’ experiences of disrespectful and abusive behavior towards women during facility based childbirth in Addis Ababa, Ethiopia. Reprod Health 15: 4.
- Kruk ME, Kujawski S, Mbaruku G, Ramsey K, Moyo W, et al. (2018) Disrespectful and abusive treatment during facility delivery in Tanzania: a facility and community survey. Health Policy Planning 33: e26-33.
- Austad K, Chary A, Martinez B, Juarez M, Martin YJ, et al. (2017) Obstetric care navigation: a new approach to promote respectful maternity care and overcome barriers to safe motherhood. Reprod Health 14: 148.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences