Abernethy Malformation- A Fresh Ray of Hope for Zatients with Diagnosis of Idiopathic Pulmonary Artery Hypertension (iPAH)
Sandeep Garg1, Prashant Bobhate2*
Department of Pediatrics, Bhaktivedanta Hospital and Research Institute, Mira Road, Mumbai , India
Department of Pediatrics, Kokilaben Dhirubai Ambani Hospital and Research center, Mumbai, India
- *Corresponding Author:
- Prashant Bobhate
Department of Pediatrics, Bhaktivedanta Hospital and Research Institute, Mira Road, Mumbai , India
Tel: 91 022 30937295
E-mail:prashantbobhate@gmail.com
Received Date: June 15, 2021; Accepted Date: October 6, 2021; Published Date: October 16, 2021
Citation: Bobhate P, Garg S(2021) Abernethy malformation- A fresh ray of hope for patients with diagnosis of idiopathic pulmonary artery
hypertension (iPAH) J Lung Vol:2 No:4.
Introduction
Idiopathic Pulmonary artery hypertension (iPAH) is generally considered a progressive disease with poor long term outcomes. But, now by diagnosing Abernathy malformation through a focused evaluation of the patient with iPAH, we can identify this potentially treatable cause, & thus improve the short and long term outcomes.1
Anatomy
Abernethy malformation (AM) also called as Extrahepatic portocaval shunt (EHPCS) is a rare anomaly of the splanchnic venous circulation. The intestinal and splenic venous blood bypasses the portal and hepatic venous system to drain directly into the systemic vein via an abnormal communication. Anatomically two types of AM have been described, type 1: End to side anastomosis with complete absence of intrahepatic portal vein and type 2: side to side anastomosis with hypoplastic intrahepatic portal veins.[1-3]
Pathophysiology
The abnormal communication results in portal blood directly flowing into the right heart thus bypassing the hepatic capillary system and physiologic hepatic clearance. This loss of hepatic clearance may result in pulmonary hypertension secondary to absence of antiangiogenic factors, endostatin and angiostatin which are involved in normal pulmonary vascular integrity.[4-5]
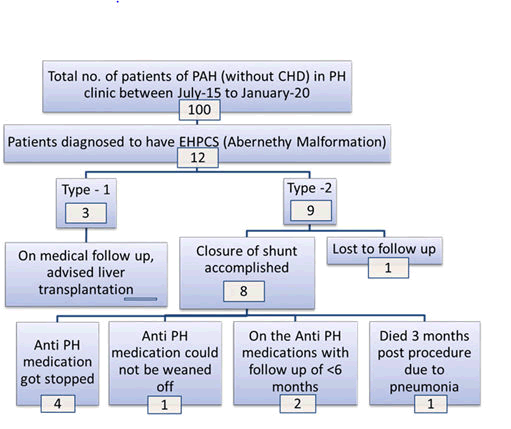
Our experience: We run a dedicated pulmonary hypertension clinic. All patients referred for evaluation of PAH undergo a battery of investigations including an ultrasound of the abdomen with portal venous Doppler (USG). Patients suspected to have EHPCS on USG underwent CT angiogram of the abdomen with portal venous phase to confirm the same and to classify the lesion.Consenting patients underwent cardiac catheterization followed by closure of the type 2 EHPCS if feasible, either by device or surgery based on anatomy and result of balloon occlusion test7. We have done a retrospective analysis of data of EHPCS and PAH. Results are summarized in flow charts below. (Figure 1)
Review of literature
EHPVC is an important and treatable cause of pulmonary hypertension. Multiple case series including our series have demonstrated that closure of EHPCS can result in decrease of pulmonary artery pressures. 3,4,5,6,7
Conclusion
Congenital portosystemic malformations form an important and potentially treatable cause of pulmonary hypertension, should be investigated in every case of iPAH (as labeled otherwise). USG abdomen with portal Doppler is the screening test. Further detailed evaluation by CT angiogram and cardiac catheterization with balloon occlusion test has been advocated to accurately assess the presence of intrahepatic portal radicals. Closure of the malformation early in the disease process can result in reduction of the PA pressure and pulmonary vascular resistance in selected patients.
References
- Hansmann G. Pulmonary hypertension in infants, children, and young adults. Journal of the American College of Cardiology. 2017; 69(20): 2551-2569.
- Knirsch W, Benz DC, Bühr P, Quandt D, Weber R, Kellenberger C, Braegger CP, Kretschmar O. Catheter interve ntional treatment of congenital portosystemic venous shunts in childhood. Catheterization and Cardiovascular Interventions. 2016; 87(7): 1281-1292.
- Sharma S, Bobhate PR, Sable S, Kumar S, Yadav K, Maheshwari S, Amin S, Chauhan A, Varma V, Kapoor S, Kumaran V. Abernethy malformation: single-center experience from India with review of literature. Indian Journal of Gastroenterology. 2018; 37(4): 359-364.
- Yi JE, Jung HO, Youn HJ, Choi JY, Chun HJ, Lee JY. A case of pulmonary arterial hypertension associated with congenital extrahepatic portocaval shunt. Journal of Korean medical science. 2014; 29(4): 604.
- Kraus C, Sheynzon V, Hanna R, Weintraub J. Single stage endovascular treatment of a type 2 abernethy malformation: successful nonsurgical outcome in a case report. Case reports in radiology. 2015; 2015.
- Stepffer C, Marques A, Barbosa JD, Ferrario S, Haag D. Pulmonary Arterial Hypertension in a Patient with a Portosystemic Shunt: Diagnostic Challenge. CASE: Cardiovascular Imaging Case Reports. 2020; 4(2): 93.
- Bobhate P, Garg S, Sharma A, Roy D, Raut A, Pawar R, Karande T, Kulkarni S. Congenital extrahepatic portocaval malformation: Rare but potentially treatable cause of pulmonary hypertension. Indian Heart Journal. 2021; 73(1): 99-103.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences