A Rare Case of Neck of Femur Fracture in A Female Adolescent Associated With Minor Trauma and Impaired Bone Metabolism
Olamide Olatokun*, Hani B Abdul-Jamar, and Thomas Nash
Department of Trauma and Orthopaedics, Northwick Park Hospital, United Kingdom
- *Corresponding Author:
- Olamide Olatokun
Department of Trauma and Orthopaedics
Northwick Park Hospital
United Kingdom
Tel: 07894300944
E-mail: olamide.olatokun@nhs.net
Received Date: November 02, 2020; Accepted Date: November 16, 2020; Published Date: November 23, 2020
Citation: Olatokun O, Abdul-Jabar HB, Nash T (2020) A Rare Case of Neck of Femur Fracture In A Female Adolescent Associated With Minor Trauma And Impaired Bone Metabolism. Endocrinol Metab Vol. 4 No.5:3.
Abstract
This report describes a rare Neck of Femur (NOF) fracture in a 17-year-old female following a fall down two steps without preceding history of pain or medical disease. She had menarche at 14 with regular cycle however BMI was 15.82. Skin was covered for cultural reasons. Pelvic radiograph confirmed right NOF fracture. Given the low-impact injury and rarity of NOF fractures in this age, extensive blood investigations were performed post operatively. Vitamin D was 2 nmol/L (50-140), calcium 1.92 mmol/L (2.20-2.60), Parathyroid Hormone (PTH) 14.2 pmol/L (1.6-6.9), phosphate 1.06 mmol/L (0.80-1.50), ALP 380 IU/L (0-187). Others were normal. She was symptomatic of hypocalcaemia, with positive Chvostek’s sign. Impression Secondary Hyperparathyroidism (SHPT) due to vitamin D Deficiency (VDD) leading to NOF fracture. Fracture was repaired and a cholecalciferol course commenced. Following discharge, DEXA scan identified lumbar bone mineral density of T-score of -2.0, signifying osteopenia. Very few cases of NOF fracture in adolescents are reported. Those reported are associated with significant trauma or with known underlying medical conditions. In this rare case, NOF fracture in an adolescent patient without prior history, later found to have impaired bone metabolism is presented. Normal bone metabolism is complex and well documented. SHPT can lead to increased bone turnover, loss and increased fracture risk. Vitamin D is vital for bone health. Here is it stressed that VDD should not be overlooked as life altering complications can follow. Early identification and supplementation is recommended. Verbal consent has been obtained and there are no conflicts of interests.
Keywords
Bone metabolism; Hypocalcaemia; Secondary hyperparathyroidism; Vitamin D deficiency
Introduction
Neck of Femur (NOF) fractures within the adolescent population is rare with only few reported cases, with adolescent defined as the age group between 11-18 years old [1]. Those occurring are associated with significant high impact trauma [2,3]. A smaller portion of adolescent NOF fractures occur in patients with underlying medical conditions [2,3].
Vitamin D is a fat soluble vitamin, vital for normal bone health [4]. Natural sunlight is the main contributing factor to maintaining vitamin D levels. Vitamin D deficiency can lead to musculoskeletal complications, such as rickets in children, osteomalacia in adults and impaired bone metabolism, and non-musculoskeletal conditions, such as cardiovascular disease and chronic pain conditions [4].
This case report draws attention to the effect of 25-hydroxyvitamin D (25(OH) D) deficiency (VDD) on bone metabolism in adolescents. Informed consent was obtained from all individual participants included in the study.
Case Report
We discuss a 17-year old Somalian female presenting with inability to bear weight and pain in the right hip following a fall down two steps. Her weight was 42.4 kg with BMI of 15.82; otherwise she had an unremarkable past medical, surgical and drug history. She did not report any prior musculoskeletal pain or abnormalities. Skin was covered for cultural reasons. She had menarche at 14 years with regular cycle. On examination the right leg was externally rotated and shortened.
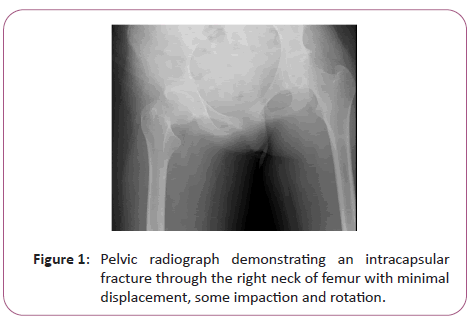
Initial blood investigations found raised ALP to 380 IU/L (0- 187), however others were within normal range (full blood count, clotting screen, remaining liver function tests, urea and electrolytes). Pelvic radiograph (Figure 1) identified a fracture through the right neck of femur.
NOF fracture was surgically repaired with cannulated screws the following day. Given the low-impact injury and rarity of NOF fractures in this age, she had extensive post-operative blood investigations. 25(OH)D was 2 nmol/L (50-140), calcium 1.92 mmol/L (2.20-2.60), Para Thyroid Hormone (PTH) 14.2 pmol/L (1.6-6.9), phosphate 1.06 mmol/L (0.80-1.50), ALP 380 IU/L (0- 187) (Table 1). She was symptomatic of hypocalcaemia, with positive Chvostek’s sign. DEXA scan was performed after hospital discharge, identifying lumbar spine Bone Mineral Density (BMD) of T-score of -2.0 signifying osteopenia [5].
| Investigation/Test | Result | Normal range |
|---|---|---|
| BIOCHEMICAL BONE PROFILE | ||
| 25-hydroxyvitamin D (nmol/L) | 2 | 50-140 |
| Alkaline phosphatase (IU/L) | 310 | 0-87 |
| Albumin (g/L) | 39 | 32-45 |
| Calcium (mmol/L) | 1.8 | 2.15-2.55 |
| Calcium-adjusted (mmol/L) | 1.92 | 2.20-2.60 |
| Phosphate (mmol/L) | 1.06 | 0.80-1.50 |
| ENDOCRINE PROFILE | ||
| Parathyroid hormone (pmol/L) | 14.2 | 1.6-6.9 |
| Thyroid stimulating hormone (mIU/L) | 2.25 | 0.51-4.30 |
| Cortisol-morning (nmol/L) | 248 | 138-690 |
| IMMUNOLOGICAL PROFILE | ||
| Immunoglobulin G (g/L) | 14.17 | 7.0-16.0 |
| Immunoglobulin A (g/L) | 2.15 | 0.5-3.5 |
| Immunoglobulin M (g/L) | 1.2 | 0.2-2.6 |
| Tissue transglutaminase antibody-IgA (U/ml) | 0.6 | 0-10 |
| Neutrophil cytoplasmic antibodies | Negative | |
| RENAL PROFILE | ||
| Sodium (mmol/L) | 141 | 133-146 |
| Potassium (mmol/L) | 4 | 3.5-5.5 |
| Urea (mmol/L) | 2.9 | 2.5-7.8 |
| Creatinine (umol/L) | 33 | 44-80 |
| Estimated glomerular filtration rate (mL/min per 1.73 m2) | >90 | |
Table 1: Post-operative blood investigation, highlighting VDD, low calcium and raised parathyroid hormone.
A suspected diagnosis of osteomalacia, severe VDD resulting in Secondary Hyperparathyroidism (SHPT) leading to osteopenia and NOF fracture was established. 20,000 units of cholecalciferol twice weekly for 6 weeks was commenced during inpatient stay followed by Adcal D3, one tablet twice daily on completion. Long term orthopaedic, endocrinology and dietary follow up are required.
Results and Discussion
Few cases of NOF fracture in children and adolescents are reported. Those reported are associated with significant trauma such as road traffic accidents and those with underlying medical conditions such as osteogenesis imperfecta, chronic kidney disease or malignancy [2,3]. Stress fractures of the femur neck have been reported in young patients involved in intense athletic activity [6]. In addition, those presenting with NOF fractures following a period of gradually worsening hip pain have been reported [6]. These aetiologies were not present in this case.
Normal bone metabolism is complex and well documented involving vitamin D, PTH and calcium [4]. 25(OH) D decreases renal calcium excretion and increases the release of calcium from bone. PTH increases intestinal absorption of calcium. In this case, the patient’s 25(OH) D was 2 nmol/L. The National Osteoporosis Society classifies VDD as 25(OH) D less than 30 nmol/L, with vitamin D insufficiency as levels between 30-50 nmol/L [7]. This patient’s 25(OH) D was not sufficient to support normal bone health. Consequently, serum calcium levels remained low and SHPT developed due to continued PTH secretion. Increased PTH leads to increased bone turnover and loss [8]. The literature has identified that those with elevated PTH and SHPT have lower BMD at the femoral neck compared to those with normal PTH levels [8], thus increasing hip fracture risk.
Vitamin D is therefore essential for bone health. VDD is becoming an increasing health concern. The British Nutrition Foundation reports that approximately 50% of the worldwide population suffer from vitamin D insufficiency [4]. Information from nationwide assessments involving the UK and USA acknowledged that adolescents in the UK had the highest prevalence of low vitamin D. These surveys identified that 40% of 11 to 18 year olds in the UK had vitamin D insufficiency, with 11-16% suffering from VDD [1].
Those particularly affected are minority ethnic groups with darker skin. One study involving GP practices based in an area of the UK, identified patients suffering from VDD. Of that cohort, just under half were of Somali origin [9]. Somali women, for example the patient presented in this case, often have skin covered for cultural reasons. NICE guidelines identify that those with darker skin and reduced exposure to sunlight are at higher risk of VDD however universal screening is only advice for patient’s presenting with symptoms suggestive of VDD such as musculoskeletal pain or on the basis of clinical need [7].
This patient was not experiencing symptoms prior to fall however 25 (OH) D levels had plummeted to only 2 nmol/L, with SHPT following as a consequence. With VDD prevalence increasing, the authors consider if current screening for VDD should include those aforementioned at risk individuals rather than waiting for symptoms to present, with aims to prevent VDD rather than treat its complications.
Our patient had low BMI however there is a constant well documented link in the literature between high, rather than low, BMI and VDD [10] therefore low BMI alone is unlikely to be the sole contributing factor to VDD in this case.
Conclusion
A rare case of a neck of femur fracture in a 17 year old female later found to have significantly impaired bone metabolism and mineralization is presented. This patient had risk factors for VDD, specifically adolescent age and dark covered skin, however did not display any clinical features prior to fall of VDD. This report therefore focuses on the importance of vitamin D levels in young at risk individuals as life altering complications can follow. Increasing screening, early identification and supplementation is therefore recommended.
References
- Cashman, K (2007) Vitamin D in childhood and adolescence. Postgrad Med J 83(978): 230-235.
- Moten M, Mussa M, Naqvi S, Kulkarni S (2017) a rare case of a non-traumatic neck of femur fracture in a 17-year-old boy associated with vitamin D deficiency. BMJ Case Rep.
- Dhar D (2013) Bilateral Traumatic Fracture of Neck of Femur in a Child: A Case Report. Mal Ortho J 7:34-36.
- Nair R, Maseeh A (2017) Vitamin D: The “sunshine” vitamin. JPJ 50:278-281.
- World Health Organization. WHO Scientific group on the assessment of osteoporosis at primary health care level.
- Lee G, Park K, Yoon T, Eshnazarovich E (2016) Bilateral Femoral Neck Stress Fracture in Child: A Case Report. Hip Pelvis 28:169-173.
- National Institute for Health and Care Excellence. Vitamin D deficiency in adults treatment and prevention.
- Di Monaco M, Castiglioni C, Tappero R (2016) Parathyroid hormone response to severe vitamin D deficiency is associated with femoral neck bone mineral density: An observational study of 405 women with hip-fracture. Hormones 15:527-553.
- Mytton J, Frater A, Oakley G, Murphy E, Barber M, et al. (2007) Vitamin D deficiency in multicultural primary care: a case series of 299 patients. BJGP57:577-579.
- Vanlint S (2013) Vitamin D and Obesity. Nutrients 5:949-956.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences