ISSN : ISSN: 2576-1455
Journal of Heart and Cardiovascular Research
A Catastrophic Case of Thromboembolism: A Case Report
Mahmoud H Abdelnaby1*, Mohamed A Ahmed2, Abdallah M Almaghraby3, Ashraf A ElAmin3 and Haitham A Badran4
1Department of Clinical and Experimental Internal Medicine, Medical Research Institute, University of Alexandria, Alexandria, Egypt
2Department of Critical Care, University of Cairo, Giza, Egypt
3Department of Cardiology, University of Alexandria, Alexandria, Egypt
4Department of Cardiology, University of Ain Shams, El-Abaseya, Egypt
- *Corresponding Author:
- Mahmoud H Abdelnaby
Cardiology and Angiology Unit
Department of Clinical and Experimental Internal Medicine
Medical Research Institute, University of Alexandria
Alexandria, Egypt
Tel: +201007573530
E-mail: Mahmoud.hassan.abdelnabi@outlook.com
Received Date: 28 February 2018; Accepted Date: 20 March 2018; Published Date: 29 March 2018
Citation: Abdelnaby MH, Ahmed MA, Almaghraby MA, ElAmin AA, Badran HA (2018) A Catastrophic Case of Thromboembolism: A Case Report. J Heart Cardiovasc Res. Vol.2 No.1:2
Copyright: © 2018 Abdelnaby MH, et al. This is an open-access article distributed under the terms of the creative Commons attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Pulmonary embolization (PE) carries a high mortality risk if not suspected and treated properly. Systemic embolization is quite common especially in cases of mobile left ventricular (LV) thrombi. We were encountered with a catastrophic case of thromboembolism with simultaneous massive PE and bilateral lower limb ischemia in a patient with biventricular systolic dysfunction and multiple LV thrombi. Tissue plasminogen activator (tPA) was given and the patient’s hemodynamics started to be stable. Unfortunately, he developed left lag, bilateral lower limb dry gangrene and subsequently he passed away despite all trials to resuscitate.
Keywords
Pulmonary embolism; Lower limb ischemia; Tissue plasminogen activator; Transthoracic echocardiography
Introduction
Pulmonary embolization (PE) carries a high mortality risk if not suspected and treated properly. Systemic embolization is quite common especially in cases of mobile left ventricular (LV) thrombi.
Case Presentation
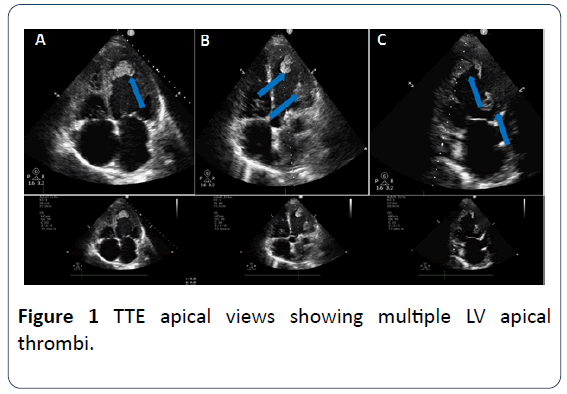
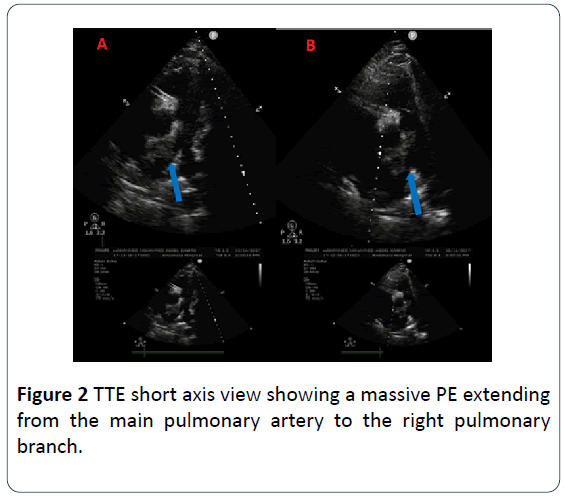
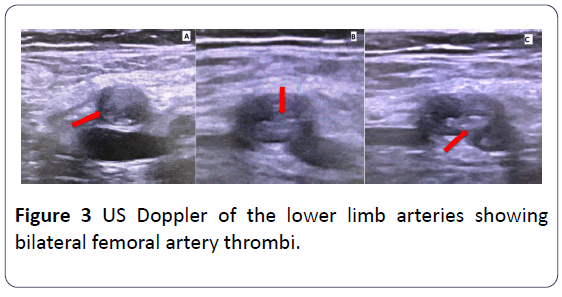
A 44 year-old-male patient with past medical history of deep vein thrombosis (DVT) and PE two months ago who wasn’t compliant on his medical therapy presented to our medical facility complaining of severe chest pain; bilateral lower limb pain and dyspnea. On clinical examination; the patient was severely distressed; hypoxic; tachycardic and in a shock state with cyanotic cold mottled lower limbs and absent distal pulsations beyond the femoral arteries with delayed capillary refilling. The patient was resuscitated in a cardiac care unit. Electrocardiogram (ECG) showed bigeminy with S1Q3T3 pattern. Urgent bedside transthoracic echocardiography (TTE) revealed bi-ventricular systolic dysfunction with multiple mobile LV thrombi and a huge thrombus at the main pulmonary artery extending to the right main pulmonary branch. There was no evidence of an intracardiac shunt by TTE. Urgent ultrasound (US) Doppler of both lower limbs’ arteries and veins showed bilateral thrombi at both femoral arteries with no distal flow and no DVT. The patient was diagnosed with acute massive PE associated with acute bilateral lower limb ischemia. A multidisciplinary approach was conducted including Cardiologists; intensivists; and vascular surgeons. Due to high-risk surgery and late presentation of lower limb ischemia which had already progressed to dry gangrene; vascular surgery had no role for any urgent interventions. The patient received tPA and vasopressors to support the hemodynamics. His hemodynamics stabilized and vasopressors were weaned but unfortunately with well-established ongoing dry gangrene of both lower limbs. Few hours later; the patient developed new dense left lag; urgent TTE revealed embolization of one of the LV thrombi. Urgent Computed tomography (CT) of the brain was unremarkable. Neurologists recommended not to start therapeutic anticoagulation; to initiate acetylsalicylic acid and to do a follow-up CT of the brain after 24 hours. Within the next 12 hours; his hemodynamics deteriorated again; with high-grade fever reaching 39-40°C which was not responding to antipyretics. Follow-up TTE revealed the same data. He didn’t respond to maximum doses of vasopressors. Later; the patient developed cardiac arrest with failure of all trials for resuscitation (Figures 1-3).
Discussion
In patients presenting with simultaneous pulmonary and systemic arterial embolization; it is important to rule out the existence of a possible patent foramen ovale (PFO) [1]. A small caliber PFO is considered hemodynamically insignificant; while larger PFOs can act as a pathway for thrombi; air; fat; vegetations from the right side to cross to the arterial circulation; causing paradoxical emboli and stroke [2]. A hypercoagulable state workup which includes tests of Factor V Leiden and prothrombin mutations; protein C and protein S deficiency; and antithrombin-III; elevation of clotting factors VIII; IX; XI; and fibrinogen and homocysteine levels; and anticardiolipin antibodies should be considered as a standard in cases of thrombosis. Work-up should be done two to four weeks after anticoagulation stoppage because acute phase of thrombosis and anticoagulation will alter the results of some of those tests. Undiagnosed malignancy must be kept in mind as a cause of the hypercoagulable state [3]. Hemodynamically unstable PE patients are candidates for treatment with IV thrombolysis or mechanical thrombectomy [4]. Streptokinase and tPA are the only agents studied so far for this indication [5] and the decision of thrombolysis must be individualized based on the patient clinical characteristics weighing the benefits and the hazards [6]. In our case thrombolysis was mandatory due to obstructive shock despite the risk of embolization of the LV thrombi and the already existing bilateral lower limb thrombosis.
Conclusion
Thromboembolism carries a high risk of morbidity and mortality so; it should be investigated thoroughly to define its etiology. Treatment must be through a multidisciplinary team approach weighing risks and benefits according to the patient’s condition in order to reduce fatal complications.
References
- Maffè S, Dellavesa P, Perucca A, Paffoni P, Paino A, et al. (2008) Pulmonary embolism associated with paradoxical arterial embolism in a patient with patent foramen ovale. Giornale italiano di cardiologia 9: 637-640.
- Buchholz S, Shakil A, Figtree GA, Hansen PS, Bhindi R (2012) Diagnosis and management of patent foramen ovale. Post Grad Med J 2011: 130368.
- Abunnaja S, Clyde M, Cuviello A, Brenes RA, Tripodi G (2014) Concomitant deep venous thrombosis, femoral artery thrombosis, and pulmonary embolism after air travel. Case Rep Vasc Med 2014: 174147.
- Weinberg I, Jaff MR (2014) Accelerated thrombolysis for pulmonary embolism : Will clinical benefit be ultimately realized? Circulation 28: 420-421.
- Chatterjee S, Chakraborty A, Weinberg I, Kadakia M, Wilensky RL, et al. (2014) Thrombolysis for pulmonary embolism and risk of all-cause mortality, major bleeding, and intracranial hemorrhage: a meta-analysis. JAMA 311: 2414-2421.
- Martin C, Sobolewski K, Bridgeman P, Boutsikaris D (2016) Systemic thrombolysis for pulmonary embolism: A review. Pharma Therapeut 41: 770.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences