A Case Study on Tetraphocomelia
Department of Pediatrics, Texas Tech Health Sciences Center, School of Medicine Amarillo, Texas, USA
- *Corresponding Author:
- William Sessions
Department of Pediatrics, Texas Tech Health Sciences Center, School of Medicine Amarillo, Texas, 79106, USA.
E-mail: William.S.Sessions@ttuhsc.edu
Received date: January 23, 2018; Accepted date: February 07, 2018; Published date: February 14, 2018
Citation: Sessions W, Nguyen D, Deitrick J, Naqvi M, Al-Zubeidi D, et al. (2018) A Case Study on Tetraphocomelia. J Birth Defects 1:1
Abstract
A newborn female presented with gross tetraphocomelia lacking features of an associated syndrome or relevant family or birth history that would cause the patient to be born with this anomaly. Tetraphocomelia is characterized by severe symmetrical limb reduction in utero. Several syndromes are associated with this finding: Robert’s syndrome, Thrombocytopenia with Absent Radius syndrome, Grebe Syndrome, Waardenber syndrome, and Holt-Oram syndrome. Furthermore, certain in utero exposures, such as thalidomide, alcohol and cocaine, are also associated with similar musculoskeletal deformations. Due to the lack of associated symptoms or significant history, our case did not fit into any specific syndrome and appears to be the result of a sporadic, non-hereditary limb deficiency involving all four limb buds. This unique presentation of a rare congenital anomaly was possibly caused by amniotic bands or a vascular accident in utero, resulting in an isolated occurrence during the critical period of limb development, between fourth and the eighth week of gestation.
Keywords
Tetraphocomelia; Sporadic limb deficiency; Congenital anomaly
Introduction
Phocomelia and amelia are incredibly rare conditions, and very little is currently known about the etiology of sporadic cases. Isidore Geobbrey St-Hilaire first described phocomelia in 1838 as an almost complete deficiency of the long bones of a limb. The term originates from “phoka” and “melos,” the Greek words for “seal” and “limb,” respectively. Thus, phocomelia literally means “seal limb” [1-8]. Amelia, on the other hand, refers to the complete absence of a limb, which may occur in isolation or in combination with multiple congenital malformations. Amelia is an uncommon congenital malformation, with an incidence of 1.5 per 100,000 live births and 7.9 per 100,000 stillbirths [4]; phocomelia has a variance in its reported incidence between 0.6 per 100,000 live births to 4.2 per 100,000 live births [9]. We report a case of a female baby with an isolated presentation of amelia and phocomelia with no other associated anomalies.
Case
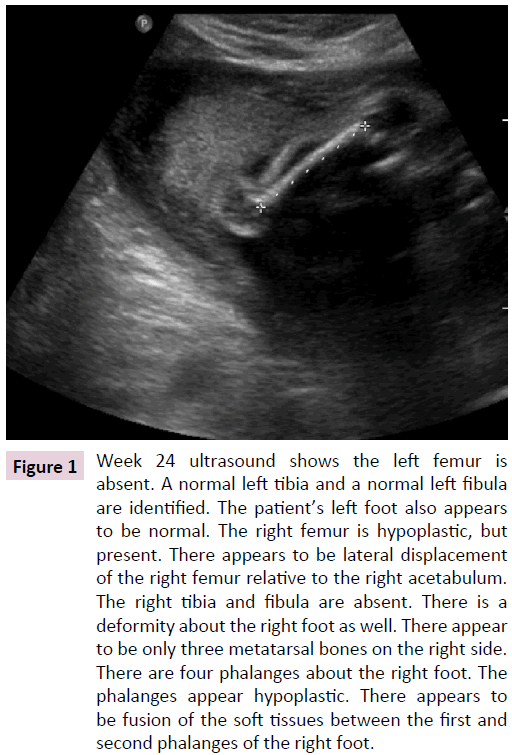
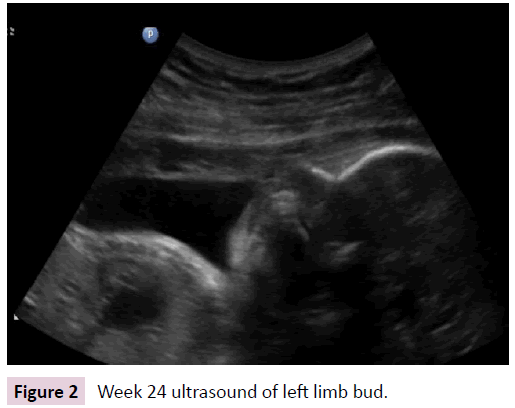
The mother of our patient was a 24 year old mother G2P1010 female who received adequate prenatal care. She took perinatal vitamins during pregnancy, but no other medications, and denied smoking, drinking alcohol, or use illicit drugs. She had history of previous spontaneous abortion for unknown reasons. On her 24 week ultrasound (Figures 1 and 2), the growth anomaly and oligohydramnios were detected with no change to her prenatal care. She had no history of consanguinity, diabetes, or any other chronic medical condition. No history of malformations was present in either parent or their extended families. The baby was delivered via C-section at 38 weeks and 6 days gestation. During the delivery, the NICU team was in attendance, and NRP guidelines were followed. The infant had Apgar scores of 3 and 9 at one and five minutes, respectively. Initial physical examination of the infant revealed that the upper limbs were absent and the lower limbs were malformed, causing direct admission to the NICU.
Figure 1: Week 24 ultrasound shows the left femur is absent. A normal left tibia and a normal left fibula are identified. The patient’s left foot also appears to be normal. The right femur is hypoplastic, but present. There appears to be lateral displacement of the right femur relative to the right acetabulum. The right tibia and fibula are absent. There is a deformity about the right foot as well. There appear to be only three metatarsal bones on the right side. There are four phalanges about the right foot. The phalanges appear hypoplastic. There appears to be fusion of the soft tissues between the first and second phalanges of the right foot.
Further examination was as follows: vital signs stable; high arched palate, intact lip and palate, no ear deformities, no eye deformities; RRR, soft murmur 2/6; no abdominal abnormalities; normal female external genitalia; alert, active and crying, primitive reflexes intact bilaterally. An echo showed a moderate patent ductus arteriosus with a positive heart murmur, which was confirmed with a color flow doppler. The doppler also showed a small left to right shunt across the patent foramen ovale site. There was no ventricular septal defect or coarctation of the aorta present. The renal, cranial and abdominal ultrasound were within normal limits. The skeletal exam revealed that both upper limbs were absent with a dimple marking their site, the left leg was abnormally short with five normal appearing digits, and the right leg was shortened with a three digit foot. Due to the obvious congenital anomalies and cardiac murmur, further workup was indicated: echo showed moderate PDA, abdominal ultrasound and neuro sonogram were normal. Chromosomal analysis revealed normal 46XX female phenotype.
After a short and largely unremarkable stay in the NICU, she was dismissed on day of life 4. She was followed up multiple times in the high risk clinic and was eventually referred to an orthopedic facility in Dallas for rehabilitation and group support. Parentphysician conference successfully facilitated acceptance and bonding between both the parents and their new baby.
Discussion
Amelia is an uncommon congenital malformation, with an incidence of 1.5 per 100,000 live births and 7.9 per 100,000 stillbirths. Tetraphocomelia, however, has an even lesser incidence and has scarce epidemiological studies [9]. This specific case is unique in that it exemplifies an individual born with tetraphocomelia but no other congenital anomalies commonly found in related syndromes. The differential diagnosis and predisposing factors are interesting points of conversation because there are a multitude of errors during embryogenesis that could bring about the tetraphocomelia.
During normal embryogenesis, a wide range of genes contribute to the normal formation of the limbs. The genes most prominent in development are the Wnt-7, Shh, and the FGF gene. Wnt-7 gene regulates the development of the ventral-dorsal axis of the limbs. The ventral-dorsal axis determines the anterior and posterior surfaces of the upper and lower limbs. In contrast, the Shh will deal with the anterior-posterior axis which will position the toes and fingers accordingly. Lastly, the FGF gene will promote distal limb growth or elongation of the limb from the body. Any error in these genes can cause shorter limbs (FGF disfunction), inappropriate location of fingers or toes (Shh), or the loss of anterior and posterior surfaces of the limbs (Wnt-7) [10,11]. On a biological level, the down regulation of these genes appears to disrupt the formation of immature blood vessels, resulting in the inability for limb growth and development [11]. Research has shown that a dose of Thalidomide as small as 50 mg between days 20 and 36 post fertilization can bring about adverse side effects in 50% of individuals. Thalidomide taken before day 20 post fertilization causes miscarriage, and exposure after day 36 has not shown to cause any defects [11]. Exposure to Thalidomide between days 20-24 causes ear and eye anomalies, exposure between days 24-31 causes upper limb anomalies and exposure between days 27-33 causes lower limb anomalies. While the exact pathogenesis of the limb disturbance witnessed in tetraphocomelia is not fully understood, the above explained mechanisms are most commonly accepted as sources for the variance from normal embryonal development.
Besides embryological errors, there are a multitude of syndromes that have phocomelia or tetraphocomelia as a symptom or association. Those syndromes include Roberts syndrome, Femur-fibular-ulnar syndrome, Thrombocytopeniaabsent radial syndrome (TAR syndrome), Okihiro Syndrome and Holt-Oram syndrome. Both Okihiro and Holt-Oram Syndrome present similar to Tetraphocomelia, but they have known genetic mutations in SALL4 and TBX5 respectively [12]. The constellation of symptoms seen with Roberts syndrome include symmetrical tetraphocomelia, cleft lip, cleft palate, microcephaly and coloboma of the eye and is known to be caused in a mutation to ESCO2 gene (Establishment of Sister Chromatid Cohesion 2 [13]. Another syndrome is Femur-fibula-ulna syndrome, which presents with absence of the proximal part of the femur and is associated with fibular ray defect, ulnar ray abnormalities and unilateral limb anomalies. Thrombocytopenia-absent radial syndrome is associated with thrombocytopenia with bilateral radial aplasia [14]. Holt-Oram syndrome is seen with cardiac anomalies frequently as ASD and upper limb deformities [2]. While our patient did not have any of the other symptoms associated with these syndromes, it is important for primary care physicians to review the related symptoms and potential causes of tetraphocomelia.
References
- Shonubi AM (2006) Asymmetrical Tetraphocomelia with Radiohumeral Synostosis. Annals of Saudi Medicine 26: 318-320.
- https://emedicine.medscape.com/article/159911-overview.
- Bermejo SE, Cuevas L, Amar E, Bianca S, Bianchi F, et al. (2011) Phocomelia: A Worldwide Descriptive Epidemiologic Study in a Large Series of Cases From the International Clearinghouse for Birth Defects Surveillance and Research, and Overview of the Literature. American Journal of Medical Genetics 4: 305-320.
- Froster-Iskenius UG, Baird PA (1990) Amelia: Incidence and Associated Defects in a Large Population. Teratology 41: 23-31.
- Fryns H, Goddeeris P, Moerman F, Herman F, Van Den Berghe E (1980) The Tetraphocomelia-Cleft Palate Syndrome in Identical Twins. Human Genetics 53: 279-281.
- https://onlinelibrary.wiley.com/doi/10.1002/(SICI)1096-8628(19971031)72:3%3C307::AID-AJMG11%3E3.0.CO;2-X/full
- George RG (1919) Transactions of the Philadelphia Academy of Surgery: State Meeting Held May 5, 1919. Annals of Surgery 70: 251-254.
- Kumar SS (2015) Tetra-Phocomelia: The Seal Limb Deformity - A Case Report. Journal of Clinical and Diagnostic Research.
- Anurag S, Chaudhary R (2016) Nonsyndromic Phocomelia: A Case Series. Translational Biomedicine 7.
- Kumar SA, Sanjay SC, Krishna L, Krishnappa N (2015) Tetra-Phocomelia: A Rarest of Rare Case. Journal of Clinical and Diagnostic Research 9: 3-4.
- Therapontos C, Erskine L, Gardner ER, Figg WD, Vargesson N (2009) Thalidomide Induces Limb Defects by Preventing Angiogenic Outgrowth during Early Limb Formation. Proceedings of the National Academy of Sciences of the United States of America 106: 8573-8578.
- Neil V (2013) Thalidomide Embryopathy: An Enigmatic Challenge. International Scholarly Research Notices.
- Hugo V, Waisfisz Q, Gordillo M, Sakai N, Yanagihara I, et al. (2005) Roberts Syndrome Is Caused by Mutations in ESCO2, a Human Homolog of Yeast ECO1 That Is Essential for the Establishment of Sister Chromatid Cohesion. Nature Genetics 37: 468-470.
- https://reference.medscape.com/article/959262-overview.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences