ISSN : 2393-8862
American Journal of Pharmacology and Pharmacotherapeutics
A Brief Introduction and Treatment Protocol of COVID-19: A Review
Mohit Goyal1*, Srishti Gosain1, Sudhakar Kaushik1 and Sakshi Garg2
1Department of Pharmaceutical Sciences, SGRR University, Dehradun, India
2Department of Health Sciences, Pt BD Sharma University of Health Sciences, Rohtak, India
- *Corresponding Author:
- Mohit Goyal
Department of Pharmaceutical Sciences, SGRR University, Dehradun, India
Tel: 8930109056
E-mail: mohitgoyal23102000@gmail.com
Received Date: December 10, 2021; Accepted Date: December 24, 2021; Published Date: December 31, 2021
Citation: Goyal M, Gosain S, Kaushik S, Garg S (2021) A Brief Introduction and Treatment Protocol of Covid 19: A Review. Am J Pharmacol Pharmacother Vol.8 No.4
Abstract
There was the emergence of a new public health crisis known as COVID-19 or SARS-CoV-2. It is thought to be originated from a microbiology research lab of Wuhan, China. This was found to be similar as of SARS [Severe Acute Respiratory Syndrome] that was there in year 2003. The symptoms of COVID-19 that were reported are headache,pyrexia, cough, sore throat, breathlessness, fatigue, malaise etc. There were a lots of different treatment protocols in practice during that time because no one knew the exact treatment of this disease. Physicians were trying to treat it symptomatically. The primary symptoms in non-serious patients were loss of smell and taste. Various antivirals have been used in this but the most effective was found to be favipiravir. There were very serious complications of COVID-19 which cannot be treated properly. In this review article author have tried to give a treatment protocol which showed good results in patients with COVID-19 and also some of the drugs are there to overcome the Side effects of some drugs used in COVID-19. The major target organ of SARS virus is lungs and an attempt is made to prevent excess damage to the lungs but in some cases, it was not achieved so the last attempt is to transplant lungs is tried in some patients and a good result is obtained.
Keywords
Treatment protocol; Lungs; COVID-19; SARS; Pyrexia; Transplant
Introduction
Recently the world faced a serious bio war against a virus named SARS-CoV-2 broadly termed as severe acute respiratory syndrome corona virus 2, also known as n-CoV or novel coronavirus [1]. This was first released by a lab of Wuhan, Hubei province, china in December 2019. It was found to be spread via nasal route in the form of droplets. As per record cases reported till date [23/05/21] are 16,63,46,635 and total deaths reported till [23/05/21] are 34,49,117 [2]. Its symptoms are similar to that of SARS which affected humans before 16 years [2003] which are fever, sore throat, headache, dry cough, dyspnea, acute respiratory distress syndrome (Table 1). This virus got spread too fast that who was compelled to declare it as ‘Pandemic’ on March 11, 2020 [3].
Corona is a self-mutating virus. It’s different strains which are found till now are [4]:
| Classification of Human Corona Virus | |
|---|---|
| HCOV-229E | Human Corona Virus 229E |
| HCOV-NL63 | Human Corona Virus NL63 |
| HCOV-HKUI | Human Corona Virus HKUI |
| HCOV-OC43 | Human Corona Virus OC43 |
| MERS-CoV | Middle East Respiratory Syndrome Corona Virus |
| SARS-CoV | Severe Acute Respiratory Syndrome Corona Virus |
| SARS-CoV-2 | Severe Acute Respiratory Syndrome Corona Virus 2 |
Table 1: Classification of human corona virus.
SARS-CoV-2 is the third corona virus that has caused severe respiratory disease in humans, originated from Wuhan, China which is spread globally in the past two decades. The first corona virus that caused severe disease was SARS which was thought to be originated from Foshan, China and resulted in the pandemic of 2002-03. The second was the Middle East Respiratory Syndrome Corona Virus [MERS] which was originated from Arabian Peninsula in 2012 [6].
SARS-CoV-2 has diameter of 60 nm to 140 nm and distinctive spikes which ranges from 9 nm to 12 nm giving the virions, the appearance of Solar Corona.
Variants of SARS-CoV-2 are [5]:
B.1.1.7 [Alpha]: This variant was first detected in the United States in December 2020. It was initially detected in the United Kingdom.
B.1.351 [Beta]: This variant was first detected in the United States at the end of January 2021. It was initially detected in South Africa in December 2020.
P.1 [Gamma]: This variant was first detected in the United States in January 2021. It was initially identified in travelers from Brazil who were tested during routine screening at an airport in Japan, in early January.
B.1.617.2 [Delta]: This variant was first detected in the United States in March 2021. It was initially identified in India in December 2020.
These variants were seen to be mutating and spreading very rapidly, which may lead to more cases of COVID-19. This rapid increase led to increase in number of patients and resources and healthcare facilities were being shorthanded day by day which led to more casualties and death rate. There was a huge demand of oxygen cylinders and medicines used for the treatment of symptoms [6].
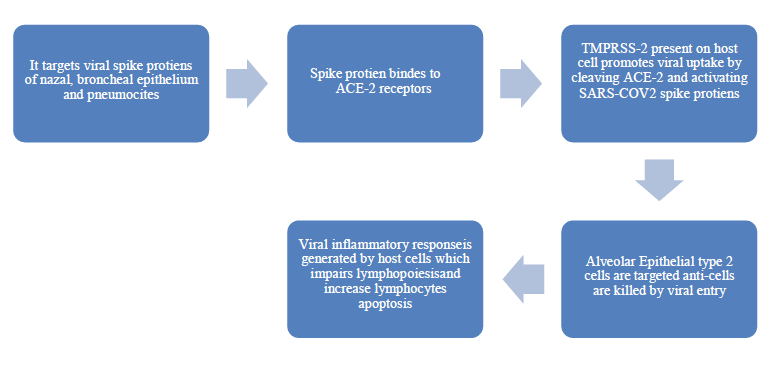
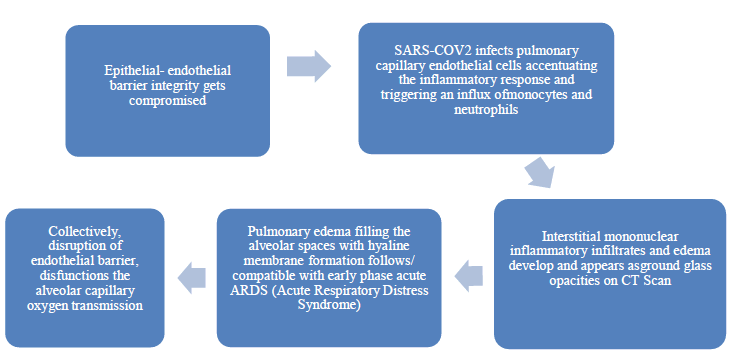
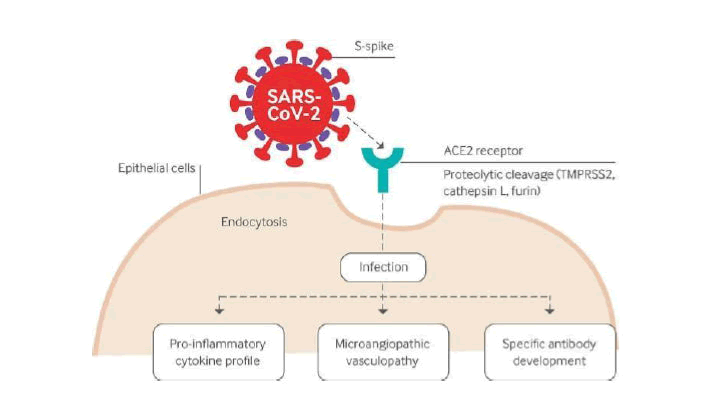
Pathogenesis of SARS-CoV-2
In later stages of infection
In severe COVID-19
• Fulminant activation of coagulation cascade and consumption of clotting factors occur which can lead to DIC [Disseminated Intravascular Coagulopathy]
• Inflamed lung tissues and pulmonary endothelial cells may result in micro thrombi formation and contribute to highincidence of thrombotic complications such as DVT, pulmonary embolism, thrombotic arterial complications, ischemia, strokes, and myocardial infarction in critically ill patients.
• The end result may be sepsis by viral infection which can be defined by multi-organ failure which is a result of dysregulations of host response to infection.
Pathogenesis of COVID-19
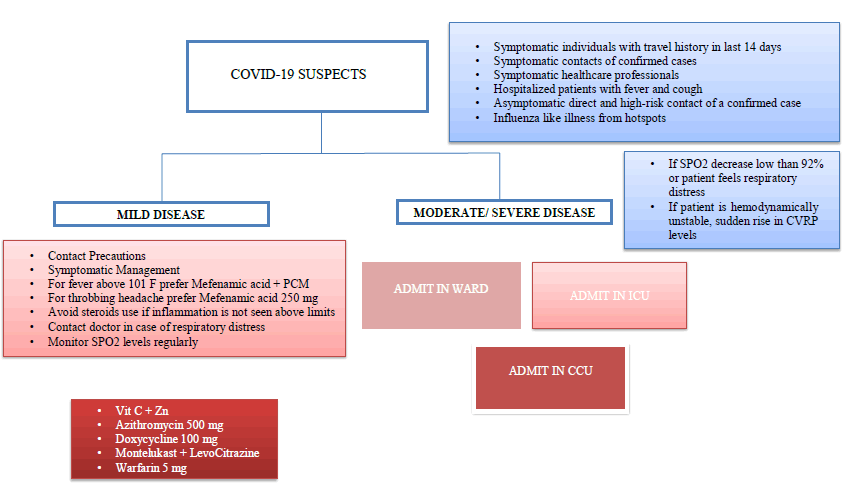
Treatment protocol for management of COVID-19
Admit in ward
• Consider HCQS 400 mg Bd for 1st day & 400 mg Od for 4 days
• Take patient on oxygen support target [92%-96%]
• Prefer non re-breathing oxygen mask
• Closely monitor serology, blood parameters & ABG [Arterial Blood Gases]
• Prefer anti-viral like: Lopinavir, Ritonavir, Fevipiravir
• Steroid’s therapy should be administered in accordance with CRP, IL-6 and other inflammatory parameters
• Start methyl prednisolone from 0.5 mg per kg to 1 mg per kg
• Low molecular weight heparin/enoxaparin should be considered in accordance with D-dimer levels
• Antibiotics like clarithromycin, clindamycin, augmenting, doxycycline should be considered
• Systemic alkalosis or acidosis should be monitored and agents like sodium citrate or phosphoric acid derivatives should be administered as per requirement of patient
• Vit B complex and Vit C should be administered for prophylaxis
• Nebulization with budesonide + levosalbutamol+ipratropium bromide
• Mucolytics can be used if patient complaints of mucus or wheezing is heard
• A janus-kinase inhibitor like: baricitinib can be used with remdesivir for better cytokine storm controlling
• Admit In ICU [SpO2 below 75%]
• Give full O2 support
• Give mechanical ventilation
• IV methyl prednisolone 1- 2 mg/kg
• Dexamethasone 6 mg bd
• Antibiotics like Feropenem/Meropenem/Vancomycin should be considered in addition to broad spectrum antibiotic like Piperacillin+Tazobactam
• IL-6 inhibitor therapy can be given in severe patients which include Ramdesivir- if SpO2 => 75% & IL- 6 is 1.85 pg/ml
• Baricitinib+Ramdesivir- for IL-6 above 1.85 pg/ml or patient with severe respiratory depression
• Immunomodulatory therapy can be administered. Example: Methotrexate, cyclosporine etc.
• C-pap or bi-pap can be used for patients with poor ventilation
• Iron exchange therapy can be given with deferoxamine, revofer and darbepoetin
• Adjunct therapy of thiamine 200 mg and Vit C 100 mg can be given
• Prophylaxis if D-dimer is high then use NTG with LMWH with close monitoring of blood pressure
• Cardiac leads should be placed permanently till the time being in ICU for cardiac monitoring
• Lactate levels should be closely monitored in order to prevent septic shock
• If lactate level does not control by single antibiotic use colistin
• For increase in IL-6 above 15 pg/ml use tocilizumab 400 mg/ itolizumab /bevacizumab
Admit in CCU
• Take patient on full life support ventilation
• Broad spectrum antibiotics and colistin can be administered
• For patients who are not responding to IL-6 inhibitors well, prefer Anakinra 100 mg
• Take patient on ECMO-ventilation [ Extracorporeal Membrane Oxygenation]
• IV steroids therapy like methyl prednisolone 2 mg/kg, hydrocortisone etc. can be used
• Mucus extraction can be done by mucus extractor
• For control of blood sugar levels, administer SC insulin
• If condition of patient is not improving, try for lungs transplant
Additional therapies target edtospecific components of the inflammatory cascades’ macrophage activation and cytokine storm modulation by inhibition of :
• IL-1 inhibitor- Anakinra [11], Canakinumab [12], Rinolacept [13]
• IL-6 inhibitors [14] - Tocilizumab, Itolizumab, Sarilumab
• Janus Kinase inhibitor [15]- Baricitinib, Tofacitinib, Ruxolitinib
• IL-5 inhibitor for asthmatic COVID-19 patients, example: Mepolizumab [16]
• TNF alpha inhibitor- Adalimumab [17], Etanercept [18], Infliximab [19]
• Inflammasome- Colchicine [20]
• IL-17 inhibitor- Brodalumab [21]
• Steroids- Prednisolone, Methylprednisolone, dexamethasone [22]
• Anticoagulants – Rivaroxaban, low molecular weight Heparin, Apixaban, Warfarin, Clopidogrel [23]
Major side effects of interleukin inhibitors
• Bone marrow depression
• Oedema
• Gi irritation
• Nausea
• Vomiting
• Loss of apatite
• Mouth ulcers [Apathoes ulcer]
• Secondary infection
• Itching
• Respiratory difficulty
Treatment for controlling possible side effects of drugs
• Furosemide: edema
• Azacytidine [25]: bone marrow depression
• Iron replacement therapy by deferoxamine and darbepoetin [26,27]
• Idaruzimab: can be used to reverse the effect of dabigatran if there is overuse of dabigatran or bleeding due to any drug side effects [28]
• IV Ig can be used to reverse the adverse effect of COVID-19 induced autoimmune disease [29]
• Amphotericin b, Caspofungin, Posaconazole can be used for mucormycosis [30]
Laboratory Tests
| LFT | KFT |
| CBC | CRP |
| D-dimer | Ferratin |
| LDH lactate | IL-6 |
| IL-1 | Blood glucose |
| Bacterial culture | Lipid profile |
| Troponin T | Troponin I |
| ANA | HR-CT |
| Chest X-Ray | CT-scan |
| MRI | CECT |
Table 2: Details of laboratory tests.
Complications of COVID-19
• It triggers autoimmune disorders like GBS [31], RA [32]
• CHF [Congestive Heart Failure] [33]
• Mucormycosis [34]
• Pneumonia [35]
• Sepsis [36]
• Kidney injury [37]
• Clotting disorders [38]
• DIC [39]
Acknowledgement
I would like to express my special thanks of gratitude to my teacher Sudhakar Kaushik who gave me this wonderful opportunity to write a review article on the current pandemic COVID-19 and its treatment protocol. He also helped me in completing this project. I came to know about so many new things. I also want to express gratitude towards my friend Srishti Gosain and my sister Sakshi Garg who helped me in completing this project on time.
Reference
- Sharma A, Tiwari S, Deb MK, MARTY JL (2020) Severe Acute Respiratory Syndrome Coronavirus -2 (SARS-CoV-2): A global pandemic and treatments strategies. IntJAntimicrobAgents
- Xu B, Gutierrez B, Mekaru S (2020) Epidemiological data from the COVID-19 outbreak, real-time case information. Sci Data 7:106
- Konala VM, Adapa S, Naramala S, Chenna A, Lamichhane S, et al. (2020) A case series of patients coinfected with influenza and COVID-19. J Investig Med
- https://www. cdc. gov/coronavirus/types. html
- https://www. cdc. gov/coronavirus/2019-ncov/variants/variant. html
- Zheng (2020) SARS-CoV-2: An emerging coronavirus that causes a global threat. Int J Biol Sci 16:1678–1685
- Reginald AMJ (Department of Nursing and Midwifery, Pentecost University). Abigail AK (Department of Nursing and Midwifery, Pentecost University). Microbiology of SARS-CoV-2 Amid School Reopening
- Yuki K, Fujiogi M, Koutsogiannaki S (2020) COVID-19 pathophysiology: A review. J Clin Immunol 215:108427
- Attaway AH, Scheraga RG, Bhimraj A, Biehl M, HatipoÄŸlu U (2021) Severe COVID-19 pneumonia: pathogenesis and clinical management. BMJ 372:436
- https://covid. aiims. edu/clinical-guidance-for-management-of-adult-COVID-19-patients
- Franzetti M, Forastieri A, Borsa N, Pandolfo A, Molteni C, et al. (2021) IL-1 Receptor Antagonist Anakinra in the Treatment of COVID-19 Acute Respiratory Distress Syndrome: A Retrospective, Observational Study. J Immunol 206:1569-1575
- Dhimolea E (2010) Canakinumab. mAbs 2:3–13
- McDermott MF (2009) Rilonacept in the treatment of chronic inflammatory disorders. Drugs Today 45:423-430
- Atal S, Fatima Z (2020) IL-6 Inhibitors in the Treatment of Serious COVID-19: A Promising Therapy? Pharmaceut Med 34:223-231
- Napolitano M, Fabbrocini G, Patruno C (2020)Potential role of Janus kinase inhibitors in COVID-19. JAAD 83:6
- Aksu K, Yesilkaya S, Topel M, Turkyilmaz S, Ercelebi DC, et al. (2021) COVID-19 in a patient with severe asthma using mepolizumab. Allergy Asthma Proc
- Fakharian A, Barati S, Mohamadi M, Dastan F (2021) Successful Management of COVID-19 with Adalimumab in a Post-Coronary Artery Bypass Graft Surgery Patient. J Cardiothora. Vasc Anesth
- Duret PM, Sebbag E, Mallick A, Gravier S, Spielmann L, et al. (2020) Recovery from COVID-19 in a patient with spondyloarthritis treated with TNF-alpha inhibitor etanercept. Ann Rheum Dis
- Stallmach A, Kortgen A, Gonnert F, Coldewey SM, Reuken P (2020) Infliximab against severe COVID-19-induced cytokine storm syndrome with organ failure-a cautionary case series. Critical Care: 24
- Lopes MI, Bonjorno LP, Giannini MC, Amaral NB, Menezes PI, et al. (2021) Beneficial effects of colchicine for moderate to severe COVID-19: a randomised, double-blinded, placebo-controlled clinical trial. RMD Open
- Pacha O, Sallman MA, Evans SE (2020). COVID-19: a case for inhibiting IL-17? Nat Rev Immunol
- Van PJ, Vos JS, Hoekstra EM, Neumann KMI, Boot PC (2020) Corticosteroid use in COVID-19 patients: a systematic review and meta-analysis on clinical outcomes. Crit Care 24:696
- Vincenzo C, Giorgio S, Riccardo R, Marco DM, Marco GM, et al. (2021) COVID-19 group, Anticoagulant treatment in COVID-19: a narrative review. Journal of Thrombosis and Thromboembolism 51:642-648
- https://www. rxlist. com/how_do_interleukin_inhibitors_work/drug-class. html
- Keating GM (2012) Azacitidine: a review of its use in higher-risk myelodysplastic syndromes/acute myeloid leukaemia. Drugs
- VelasquezJ,WrayAA(2021)Deferoxamine.In:StatPearls.TreasureIsland(FL):StatPearlspublishing
- Ibbotson T, Goa KL (2001) Darbepoetin alfa. 61:2097-2104; discussion 2105-2106
- Ibbotson T, Goa KL (2001) Darbepoetin alfa. 61:2097-2104; discussion 2105-2106
- Pollack CV Jr, Reilly PA, Eikelboom J, Glund S, Verhamme P, et al. (2015) Idarucizumab for Dabigatran Reversal. N Engl J Med 6:511-520
- Shoenfeld Y, Katz U (2005) IV Ig therapy in autoimmunity and related disorders: our experience with a large cohort of patients. Autoimmunity 38:123-137
- Song G, Liang G, Liu W (2020) Fungal co-infections associated with global COVID-19 pandemic: a clinical and diagnostic perspective from China. Mycopathologia
- Sedaghat Z, Karimi N (2020) Guillain Barre syndrome associated with COVID-19 infection: A case report. J Clin Neurosci
- Basu-Ray I, Almaddah Nk, Adeboye A (2021) Cardiac Manifestations of Coronavirus (COVID-19) In: StatPearls (Internet). Treasure Island (FL)
- Favalli EG, Ingegnoli F, De Lucia O, Cincinelli G, Cimaz R, et al. (2020) COVID-19 infection and rheumatoid arthritis: Faraway, so close! Autoimmun Rev
- Sharma S, Grover M, Bhargava S, Samdani S, Kataria T Post coronavirus disease mucormycosis: a deadly addition to the pandemic spectrum. J Laryngol Otol
- Pfeifer M, Hamer OW (2020) COVID-19-Pneumonie. Internist (Berl) 61:793-803
- Beltrán GJ, Osca VR, Pallardó FV, Ferreres J, Rodríguez M, et al. (2020) Sepsis and Coronavirus Disease 2019. Critical Care Medicine, Publish Ahead of Print
- Doherty TM, Kelley A (2020) Bleeding Disorders. In: StatPearls (Internet). Treasure Island (FL): StatPearls Publishing
- Nogueira SÁR, Oliveira SCS, Carvalho AFM, Neves JMC, Silva LSVD, et al. (1992) Renal changes and acute kidney injury in covid-19: a systematic review. Rev Assoc Med Bras
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences