Abstract
Vascular Dementia 2019: A new hypothesis on the etiology to dementia in traumatic brain injury and stroke- Hans von Holst- Karolinska University Hospital, Sweden
Increased intracellular water content defined as cytotoxic brain tissue edema is a serious secondary clinical complication to traumatic brain injury (TBI) and stroke and without the knowledge to the etiology. Recently, a hypothesis to the nervous tissue edema was presented suggesting that external dynamic and internal mechanical static impact forces caused protein unfolding resulting in an increased brain tissue water content and what happens with the metabolism in the long run. The hypothesis was confirmed by computer simulation tests. In this laboratory study, we further evaluated the hypothesis by using the mature protein laminin LN521 upon the effects of both dynamic as well as static impact forces, respectively. The treated laminin solutions were then analyzed with denatured electrophoresis and electron microscopy showing aggregation and fragmentation of the laminin structures. The present laboratory results confirm earlier hypothesis and computer simulation suggest for the first time that dynamic impact force in an accident and increased mechanical static force in stroke unfold mature proteins having the potential to increase the intracellular water content defined as cytotoxic brain tissue edema. The clinical condition resembles the phenomenon when elasmobranchs including white sharks prevent their cells from too high hydrostatic pressure in the deep sea. Thus, the present laboratory study results and knowledge from marine physics may be considered to improve the clinical treatment and outcome of TBI and stroke patients. This opens up novel perspectives how vascular dementia in TBI & stroke should be looked upon when it comes to clinical treatment. blem. Cytotoxic brain tissue edema, which is found in both grey and white matter cells, is a complicated secondary consequence to ischemic injury following cerebral diseases such as traumatic brain injury (TBI) and stroke. To some extent the pathophysiological mechanisms are known, how far from complete. A novel hypothesis regarding the etiology to cytotoxic brain edema is presented. The hypothesis is that external energy due to TBI and internal energy due to mechanical forces following stroke results in the disruption of non-covalent and covalent bonds in protein and nucleotide structures. The unfolded proteins attract water molecules while the disruption of nucleotides such as adenosine-tri-phosphates causes a dysfunction in ion hemostasis & which may tentatively explain the etiology to cytotoxic edema. Our studies using computer models shows that the kinetic energy following an impact to the head has the potential to break the chemical bonds in the protein & nucleotide structures resulting in cytotoxic brain tissue edema. Since folding of mature proteins is very much dependent on normal energy supply, the protein synthesis cannot continue during the ischemic process. Under such conditions very little of the energy rich ATP can be produced and which may result in disturbance between extra- and intra-cellular ion metabolism. The present hypothesis has the potential to develop novel drugs for therapeutic use. In order to perform their normal physiological functions, it is important that cells maintain the intracellular pH within the physiological range. Intracellular enzyme activity, cytoskeleton component integration & cellular growth and differentiation rates are all closely associated with the intracellular pH. It has been demonstrated that in nervous system diseases, such as ischemic stroke, traumatic brain injury, epilepsy, Parkinson's disease & Alzheimer's disease (AD), the common characteristics are decreased pH or acidosis at both tissular and cellular levels. Particularly, some AD-associated enzymes will have altered activities under acidic conditions. We inferred that aging or ischemia may cause intracellular acidification. This acidification not only induces apoptosis but also substantially alters enzyme activities and promotes the development of AD or vascular dementia. The hypothesis of an intracellular pH role in sporadic AD or vascular dementia will be discussed in this paper. If confirmed, this hypothesis may lead to the formulation of novel pathogenesis and novel therapeutic approaches to AD or vascular dementia. Alzheimer’s disease (AD) and traumatic brain injury (TBI) are both significant clinical problems characterized by debilitating symptoms with limited available treatments. Interestingly, both neurological diseases are characterized by neurovascular damage. This impaired brain vasculature correlates with the onset of dementia, a symptom associated with hippocampal degeneration seen in both diseases. We posit that vascular damage is a major pathological link between TBI & AD, in that TBI victims are predisposed to AD symptoms due to altered brain vasculature; vice versa, the progression of AD pathology may be accelerated by TBI especially when the brain insult worsens hippocampal degeneration. Our hypothesis is supported by recent data reporting expedited AD pathology in presymptomatic transgenic AD mice subjected to TBI. If our hypothesis is correct, treatments targeted at repairing the vasculature may prove effective at treating both diseases and preventing the evolution of AD symptoms in TBI victims. Alzheimer’s Disease (AD) affects over five million people each year in the United States. In most cases, symptoms emerge after the age of sixty, and progress on a spectrum of three stages. Memory loss and poor judgment are among the most prominent early signs and symptoms. AD is a neurodegenerative disorder primarily tied to the hippocampus region of the brain with patients exhibiting an inability to communicate and a lack of control of bowel and bladder. As the disease progresses, brain tissue in the surrounding hippocampal areas undergoes similar neurodegeneration, characterized by aberrant tau and amyloid protein deposits. AD is a debilitating, irreversible brain condition that eventually leads to death.
Author(s): Hans von Holst
Abstract | PDF
Share This Article
Google Scholar citation report
Citations : 8
Journal of Cognitive Neuropsychology received 8 citations as per Google Scholar report
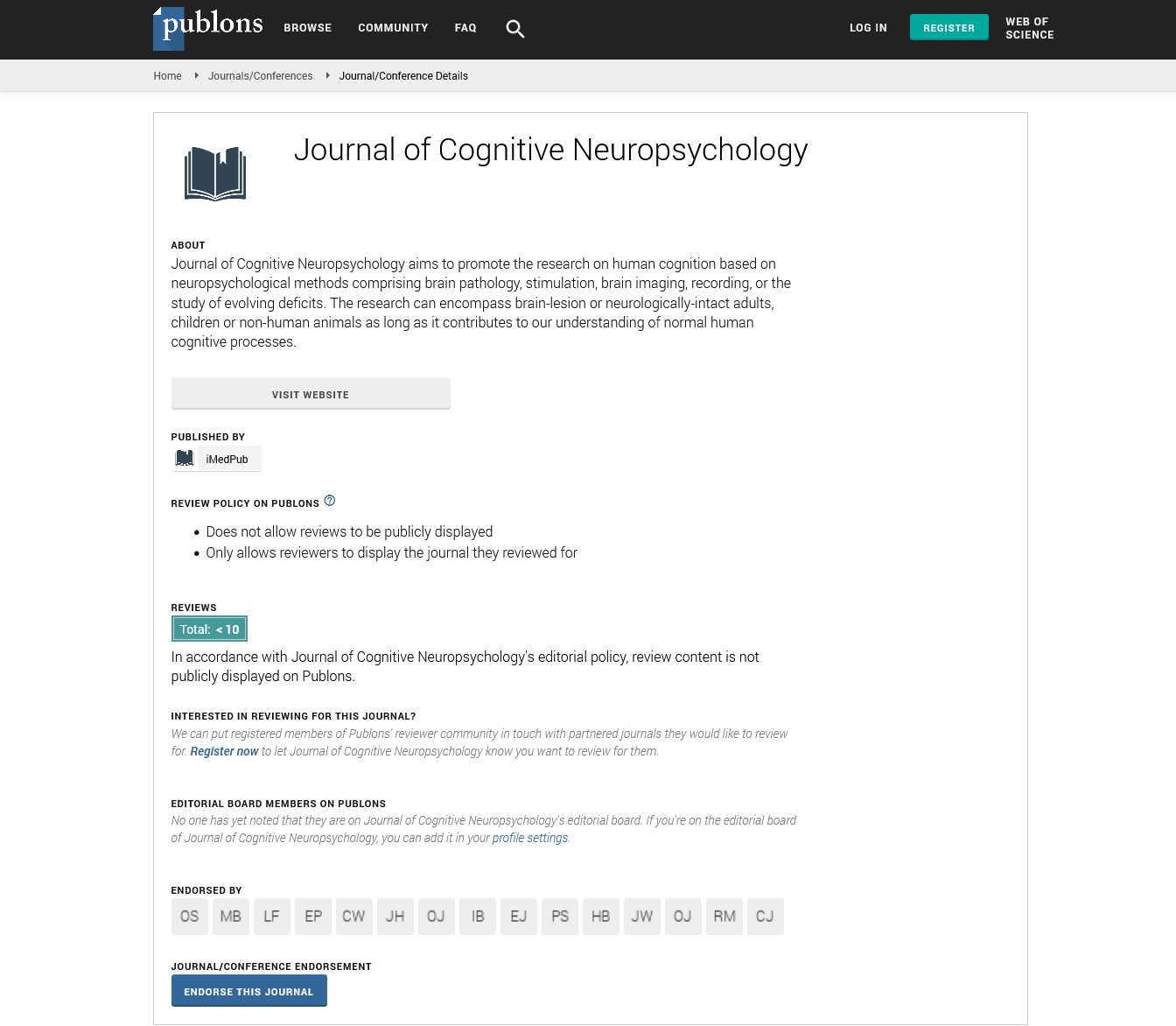
Journal of Cognitive Neuropsychology peer review process verified at publons
Abstracted/Indexed in
- Google Scholar
- Publons
- MIAR
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences