Abstract
The Influence of Pharmacological Osteoporosis Treatment on Refractures Following Kyphoplasty.
The aim of this study was to examine the relationship between pharmacological osteoporosis treatment on the refracture rate in patients who have had a thoracic or lumbar level kyphoplasty. A kyphoplasty was a non-invasive vertebral augmentation surgery used to treat compression fractures. It was a known fact that a kyphoplasty could cause future compression fractures at the levels above and below the initial procedure. In addition, spinal compression fractures were considered to be osteoporotic fractures. A single center observational cohort study with 192 patients who had kyphoplasty from 2015 until 2019 was conducted. The cohort was divided into two groups with a 1:1 ratio. The two groups were labeled Group I (pharmacological osteoporosis treatment) and Group II (no pharmacological osteoporosis treatment). Refracture was defined as having at least one future osteoporotic compression fracture requiring a kyphoplasty after the initial. Patients that had a subsequent fracture following the initial kyphoplasty procedure were placed into the “Post Kyphoplasty Refracture” (PKR) category, whereas those that didn’t have a fracture subsequent to the initial kyphoplasty were categorized as “No Post Kyphoplasty Refracture” (NPKR). 44 patients self-reported the intent to start osteoporosis treatment with their Primary Care Provider and were placed in an Intended to Treat Group (ITT). A Chi Square Independence Test was used to analyze the data. There was a significant reduction in the refracture rate (X2=4.4045, p=0.036). In Group I, the ITT group were the only patients who were lost to follow up. 0 were lost to follow up in Group II. The Chi Square Independence Test suggested a strong dependent relationship between pharmacological osteoporosis treatment and the refracture rate following kyphoplasty and determined significance in data. This study gave physicians a treatment method to reduce the chance of patients developing future compression fractures. Thus, leading to far less future kyphoplasty procedures
Author(s): Imran Alam
Abstract | PDF
Share This Article
Google Scholar citation report
Citations : 131
Journal of Surgery and Emergency Medicine received 131 citations as per Google Scholar report
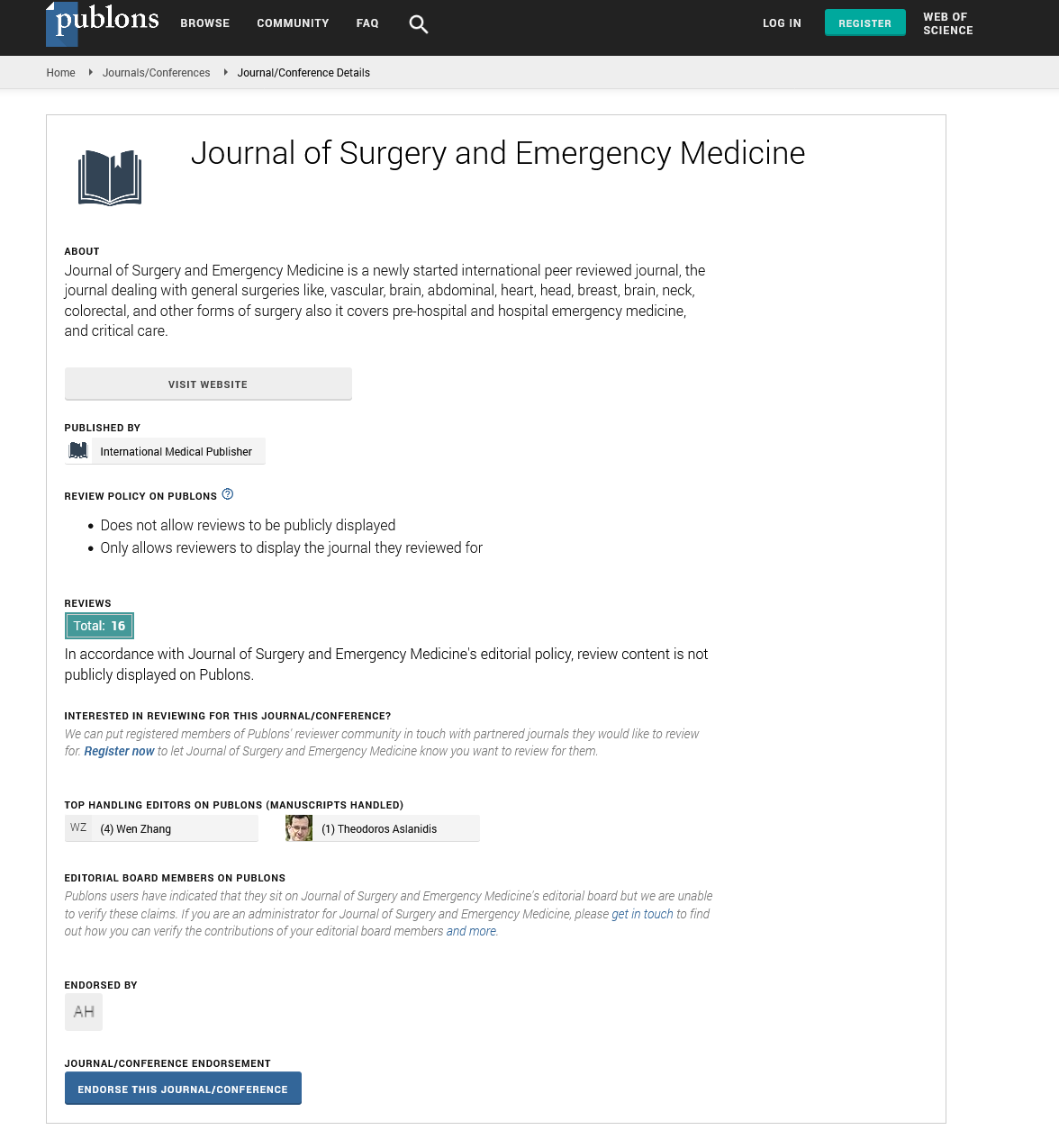
Journal of Surgery and Emergency Medicine peer review process verified at publons
Abstracted/Indexed in
- Google Scholar
- Publons
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences