Abstract
Prognostic Impact of Preoperative Prognostic Nutritional Index In Resected Advanced Gastric Cancer: A Multicenter Propensity Score Analysis.
Background:
Advanced gastric cancer (AGC) causes debilitating malnutrition and leads to deterioration of the immune response. However, the concept of the prognostic nutritional index (PNI) is controversial when applied to patients with AGC. The aim of the present study was to evaluate the effect of the PNI after gastrectomy in patients with AGC. Materials and Methods: A multicenter retrospective study was conducted using propensity score matching (PSM) in gastric adenocarcinoma patients who underwent resection via laparoscopic or open surgery between 2014 and 2017. To overcome selection bias, we performed 1:1 matching using 5 covariates.
Results: The resection margins (P<0.001) and LNM (P=0.004) were significantly different between the two groups. In univariate analysis, poor tumor differentiation (P=0.038) (R1+R2, P=0.004), vascular and neural invasion (P<0.001), and a PNI<50 (P<0.001) were associated with poor recurrence-free survival (RFS). In multivariate analysis, a PNI<50 (hazard ratio (HR), 12.993; P<0.001) was a risk factor for RFS. Univariate analysis for overall survival (OS) revealed that a PNI<50 (P<0.001) (R1+R2,P=0.006) and vascular and neural invasion (P<0.001) were risk factors. In subsequent multivariate analysis, a PNI<50 (HR, 24.501; P<0.001) was a significant risk factor for OS. Clinical assessments performed during a 12.34 (±5.050) month follow-up revealed that OS (P<0.001) and RFS (P<0.001) were worse in patients with a low PNI (<50) than in matched patients with a high PNI.
Conclusion: A low PNI is a strong predictor of unfavorable RFS and OS in patients with AGC.
Author(s): Alpha I. Balde
Abstract | Full-Text | PDF
Share This Article
Google Scholar citation report
Citations : 131
Journal of Surgery and Emergency Medicine received 131 citations as per Google Scholar report
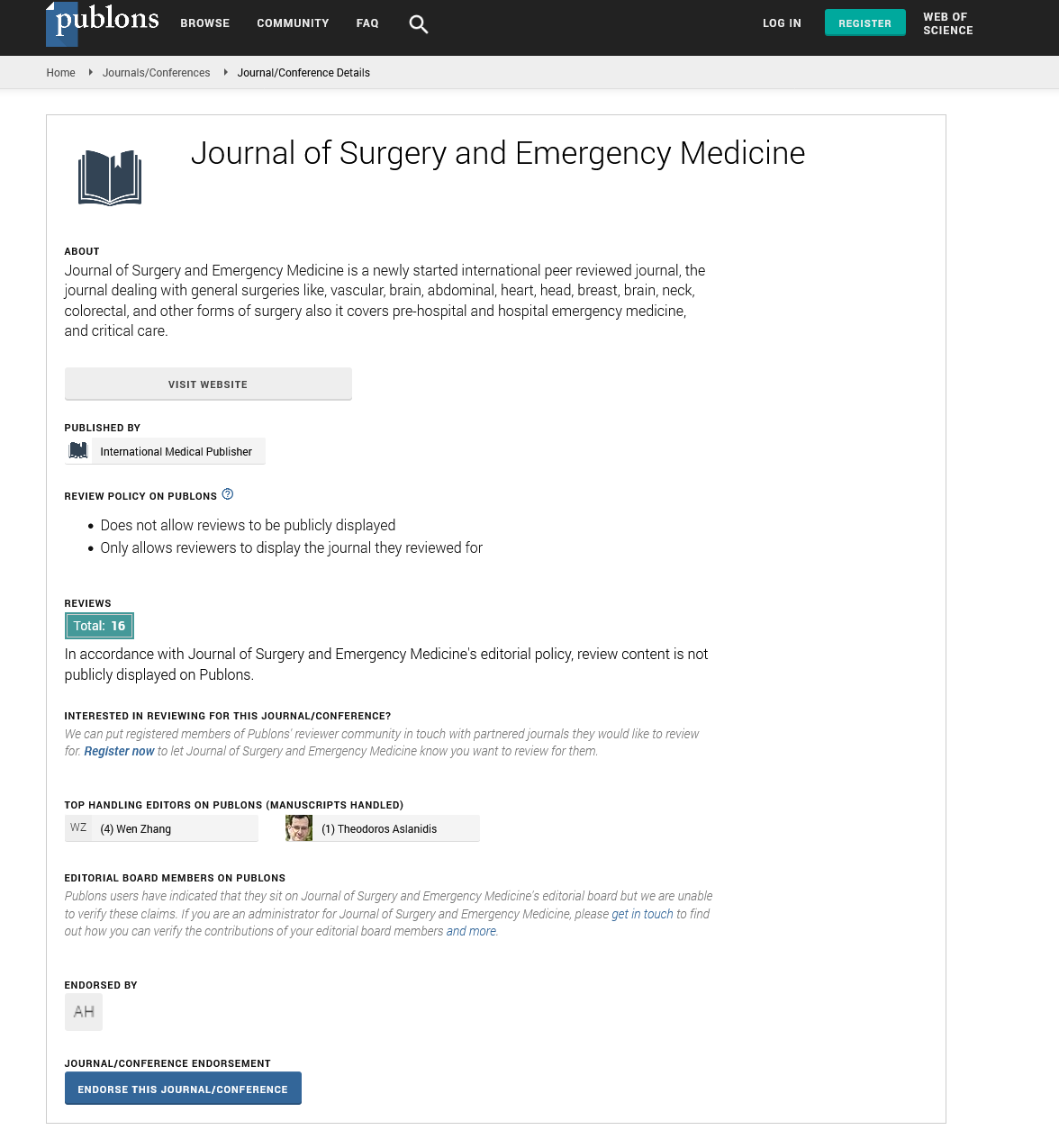
Journal of Surgery and Emergency Medicine peer review process verified at publons
Abstracted/Indexed in
- Google Scholar
- Publons
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences