Abstract
Laparoscopic subtotal cholecystectomy for difficult gallbladders: A lifesaving bailout or an incomplete operation?
Introduction: Laparoscopic Subtotal Cholecystectomy (LSTC) is a bailout procedure that is undertaken when it is not safe to proceed with a laparoscopic total cholecystectomy due to dense adhesions in Calot’s triangle. The main aim of this review was to understand the early (≤30 days) and late (> 30 days) morbidity and mortality of LSTC.
Methods: A literature review of PUBMED (Medline), Google scholar and EMBASE was conducted from 1985 to December 2020 to identify all studies on LSTC. A systematic review was then performed.
Results: 45 studies were identified, with a total of 2166 patients. Mean age was 55 +/- 15 years with 51% females; 53% (n=390) were elective procedures. The conversion rate was 6.2% (n=135). Most common indication was acute cholecystitis (n=763). Different techniques were used with the majority having a closed cystic duct/gallbladder stump (n=1188, 71%). The most common closure technique was intracorporeal suturing (53%) followed by endoloop closure. There were a total of four, 30-day mortality in this review. Early morbidity (≤30 days) included bile duct injury (0.23%), bile leak rates (18%), intra-abdominal collection (4%). Reoperation was reported in 23 patients (1%), most commonly for unresolving intra-abdominal collections and failed ERCP to control bile leak. Long term follow-up was reported in 30 studies with a median follow up period of 22 months. Late morbidity included incisional hernias (6%), CBD stones (2%), and symptomatic gallstones in 4% (n=41) with 2% (n=22) requiring completion of cholecystectomy.
Conclusion: LSTC is an acceptable alternative in patients with “difficult” Calot’s triangle.
Author(s): Mohamed Abouelazayem
Abstract | Full-Text | PDF
Share This Article
Google Scholar citation report
Citations : 131
Journal of Surgery and Emergency Medicine received 131 citations as per Google Scholar report
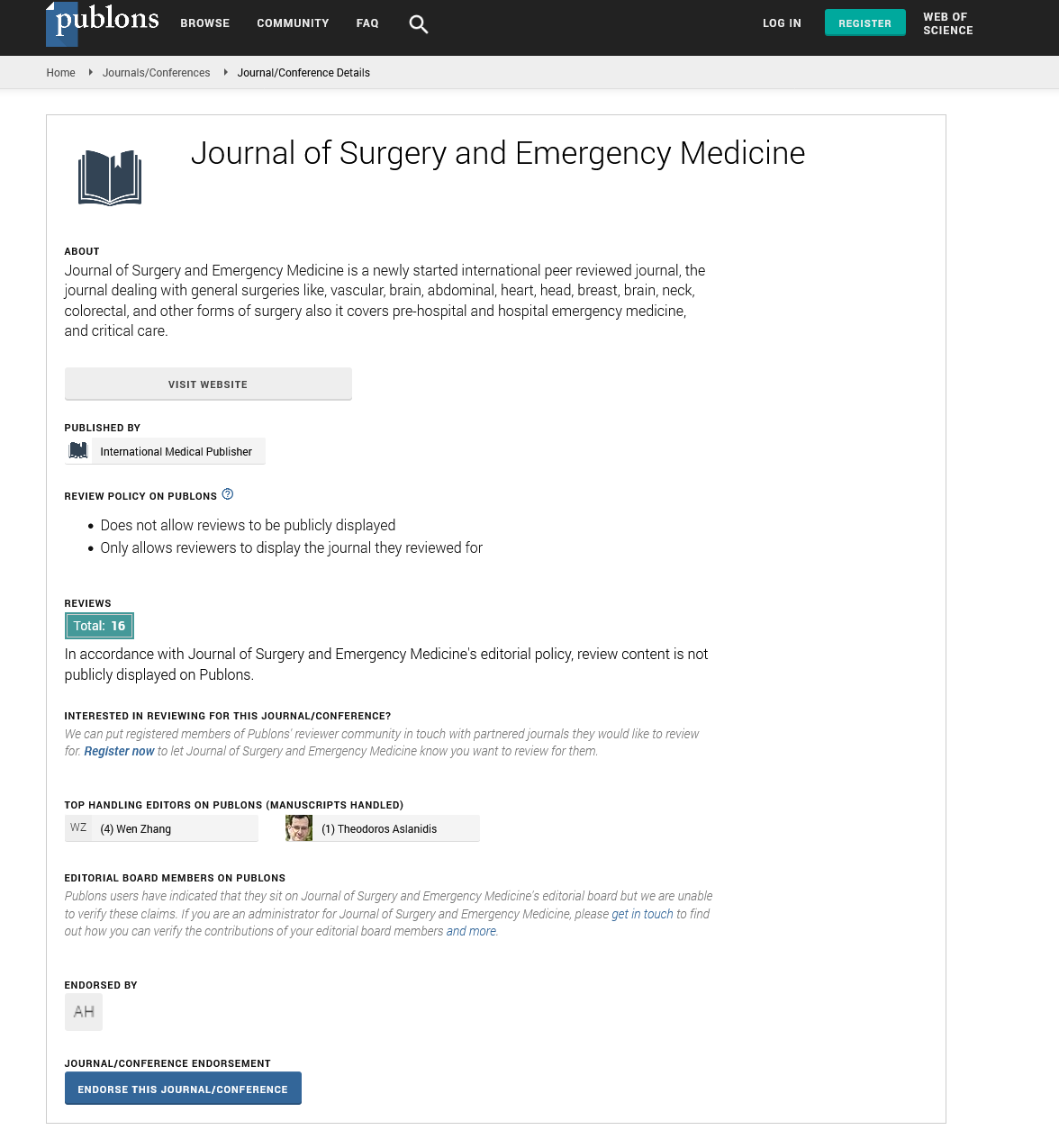
Journal of Surgery and Emergency Medicine peer review process verified at publons
Abstracted/Indexed in
- Google Scholar
- Publons
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences