Abstract
A rare case of a non-traumatic double gastric perforation
Many cases of acute abdominal pain lead to emergency hospital admissions, a large proportion of which have impending or already perforated hollow viscus, rendering an acute abdomen secondary to a ruptured viscus one of the most common surgical emergencies. The two most common pinpointed initiating factors of a ruptured viscus are Helicobacter pylori infection and chronic non-steroidal anti-inflammatory drug or steroid abuse. This case report details the occurrence of double gastric perforation in a middle-aged man who was a known heavy smoker and alcoholic beverage drinker, with no elicited history of NSAID abuse, and with questionable history of illicit drug use. Multiple peptic perforations are a relatively rare entity, much more double gastric perforations, outside the context of a traumatic event. The challenge posed by this case is the lack of literature that would confirm if the predisposing factors that contribute to the development of multiple peptic perforations are the same as those that initiate perforations specifically located within the borders of the stomach. A validation study would prove to be helpful in the management and further work-up of a double gastric perforation as well as in assessing if current therapeutic guidelines of peptic perforations are applicable precisely to multiple gastric perforations. The rare nature of this case can provide an impetus in the study of non-traumatic double gastric perforations, especially since the strongest predisposing factors identified in multiple peptic perforations – H. pylori infection and chronic NSAID use – were both absent in this patient.
Author(s): Czarsteine Sybil P. Moleño
Abstract | PDF
Share This Article
Google Scholar citation report
Citations : 131
Journal of Surgery and Emergency Medicine received 131 citations as per Google Scholar report
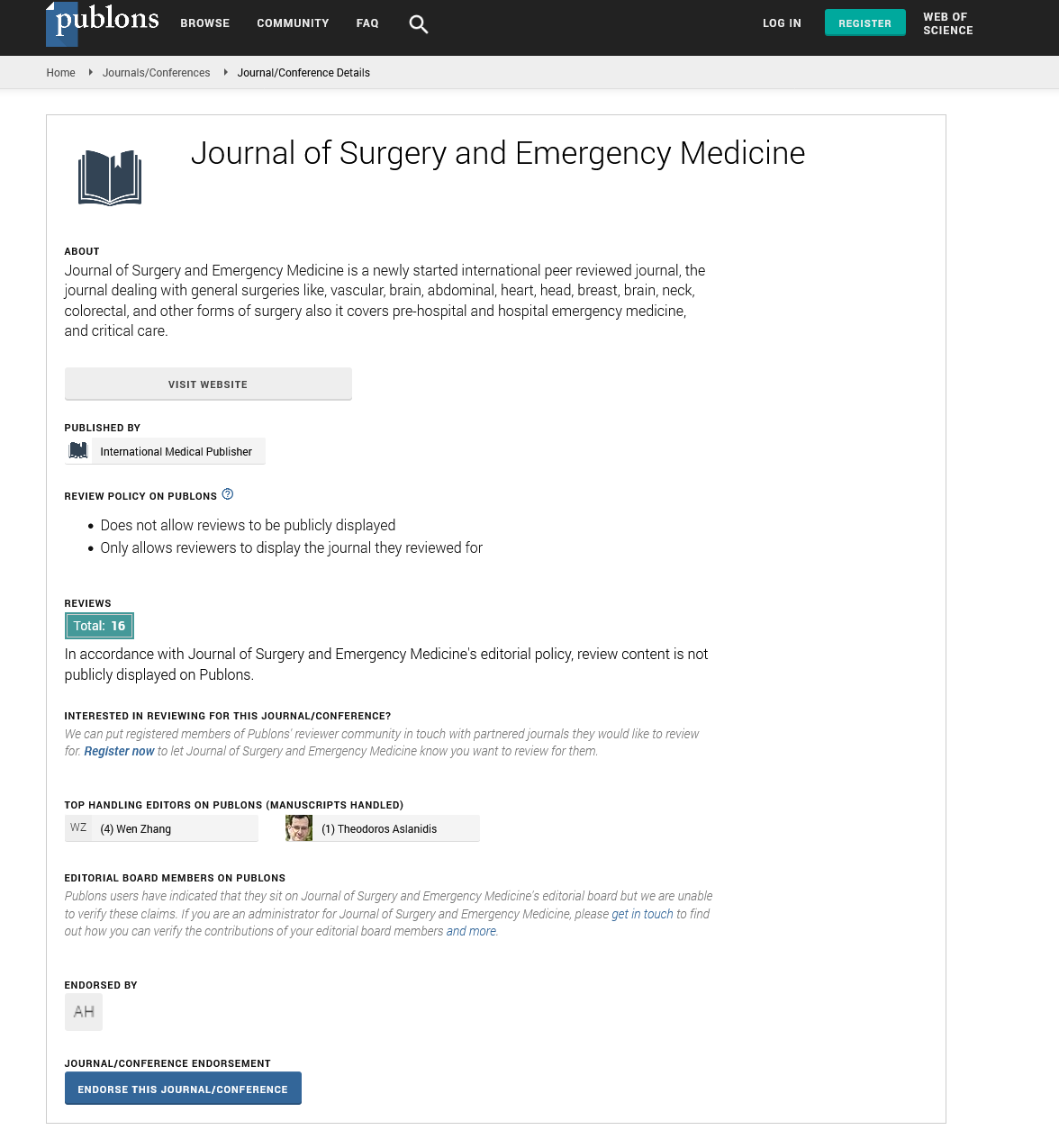
Journal of Surgery and Emergency Medicine peer review process verified at publons
Abstracted/Indexed in
- Google Scholar
- Publons
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences