Glucose-lowering Effect for Low Carbohydrate Diet (LCD) in Diabetic Patients with Positive Glutamic Acid Decarboxylase Antibody (GADA)
2Japan Low Carbohydrate Diet Promotion Association, Kyoto, Japan
3Department of Medical Research, Tokushima University, Tokushima, Japan
4Muneta Maternity Clinic, Chiba, Japan
5Department of Gastroenterology and Oncology, Institute of Biomedical Sciences, Tokushima University Graduate School, Tokushima, Japan
6Anti-Aging Medical Research Center, Graduate School of Life and Medical Sciences, Doshisha University, Kyoto, Japan
- Corresponding Author:
- Hiroshi Bando, MD
Department of Medical Research
Tokushima University, 1-61
Tokushima 770-0943, Japan
Tel: +81-90-3187-2485
E-mail: pianomed@bronze.ocn.ne.jp
Received Date: 23 April 2019; Accepted Date: 14 May 2019; Published Date: 23 May 2019
Citation: Ebe K, Bando H, Muneta T, Bando M, Yonei Y (2019) Glucose-lowering effect for low carbohydrate diet (LCD) in diabetic patients with positive glutamic acid decarboxylase antibody (GADA). Endocrinol Metab Vol. 3 No.1: 115.
Copyright: © 2019 Ebe K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Authors and collaborators have continued clinical research for Low Carbohydrate Diet (LCD) and Calorie Restriction Diet (CRD), glucose variability and M value. We investigated patients with Type 2 Diabetes Mellitus (T2DM) with positive Glutamic Acid Decarboxylase Antibody (GADA).
Subjects and methods: Subjects were 12 patients with T2DM showing positive GADA (group 1). They were given CRD on day 1,2, and LCD on day 3-14. Daily profile of blood glucose was measured each day, and data were calculated to M value expressing average glucose and Mean Amplitude of Glycemic Excursions (MAGE). Further, 12 T2DM cases with negative GADA were recruited, who were age-, sexglucose- related data-matched (group 2).
Results: Data of group 1 were as follows: age 54.9 ± 14.3 yo, HbA1c 7.1 ± 0.9%, average blood glucose and M value on day 2 vs 4 were 187 (157-255) vs 145 (114-172), 76.9 (45.9-278) vs 27.2 (19.3-83.5), respectively. In group 2, M value on day 2 vs 4 were 69.9 (37.8-149) vs 5.8 (3.5-13.3), respectively. Group 1 showed insufficient decreased glucose in M value.
Discussion and conclusion: These results suggested that cases with positive GADA would have insufficient insulin secretion in response to LCD, and may lead to Slowly Progressive Insulin-Dependent Diabetes Mellitus (SPIDDM) status in the future.
Keywords
Glutamic acid decarboxylase antibody (GADA); Slowly-progressive type 1 diabetes (SPIDDM); Glucose variability Type 2 diabetes mellitus (T2DM); M value Low Carbohydrate Diet (LCD)
Abbreviations
GADA: Glutamic Acid Decarboxylase Antibody; MAGE: Mean Amplitude of Glycemic Excursions ; SPIDDM: Slowly-Progressive Type 1 Diabetes; T2DM: Type 2 Diabetes Mellitus; LCD: Low Carbohydrate Diet; CRD: Calorie Restriction Diet; HOMA-R: Homeostasis Model Assessment of Insulin Resistance; HOMA-β: Homeostasis Model Assessment of β Cell Function
Introduction
Diabetes has caused various influences to diabetic patients with microvascular and macrovascular complications, and with their Activities Daily Living (ADL) and Quality of Life (QOL) [1]. Furthermore, diabetes has been recently one of the crucial medical problems worldwide. The number of the diabetic patients has been increasing in both of developed and developing countries. Then, the diagnosis and treatment for diabetes has been crucial in the light of social and economic aspects [2].
Diabetes has some categories including Type 1 Diabetes Mellitus (T1DM), Type 2 Diabetes Mellitus (T2DM) and others. As recent topic, there is a subtype between T1DM and T2M, which has been in focus from clinical and immunological points of view. It is necessary for careful evaluation, treatment and following up for years.
T1DM has been classified into 2 types due to the guidelines of the World Health Organization (WHO) and the American Diabetes Association (ADA) in European and North American region. They include i) Autoimmune diabetes (type 1A) and ii) Idiopathic diabetes (type 1B) [3]. Among them, type 1A is characterized for its presence of autoantibodies at the onset of hyperglycemia, such as Glutamic Acid Decarboxylase Antibody (GADA) and anti-Insulinoma-Associated Antigen 2 (IA2) and others [4]. In contrast, type 1B has been known by the dependence without the present evidence of autoimmunity [3].
On the other hand, in Japan, T1DM has been classified into rather detail way by Japan Diabetes Association (JDA). There are i) autoimmune, ii) idiopathic from the etiology aspect, and iii) acute, iv) Slowly Progressive Insulin-Dependent Diabetes Mellitus (SPIDDM), v) fulminant in the light of onset style from clinical aspect [5]. Diabetic cases with SPIDDM usually do not show ketosis or ketoacidosis at the onset, and either not require insulin treatment in earlier years [6]. As for the diagnosis of SPIDDM, there are positive results for GADA and/or some kinds of Islet Cell Antibodies (ICAs) [7].
Concerning this type of diabetic pathophysiological situation, it is called as SPIDDM in Japan and Latent Autoimmune Diabetes in Adults (LADA) in Western countries [8]. SPIDDM has been characteristic for its positive GADA and ICA. Patients with SPIDDM usually show insulin independent condition at the onset period in early years. However, within several years, the patient would possibly become insulin-dependent because of gradually impaired insulin secretion [9]. Consequently, clinical manifestation of diabetic condition has been found in SPIDDM and LADA.
For the patients with SPIDDM, T2DM and T1DM, the authors have continued clinical diabetic research for long years. Especially, we have reported comparative study of nutritional therapy, such Calorie Restriction Diet (CRD) and Low Carbohydrate Diet (LCD).
CRD had been the ordinary nutritional therapy way formerly. However, Atkins and Bernstein initiated and developed LCD during 1980-90’s in western countries [10,11]. Thus, LCD has been gradually popular, and the efficacy of LCD for weight reduction and glucose lowering has been reported and known widely. As a result, LCD revealed predominant effects in comparison with the Mediterranean and CRD in the Dietary Intervention Randomized Controlled Trial (DIRECT) study [12,13]. There have been various discussion on CRD and LCD so far, indicating clinically predominance of LCD [14,15].
In contrast, authors and co-workers have initiated LCD for the first time in Japan [16]. Successively, we have developed three types of simple application of LCD into clinical practice and health care field, which are petite LCD, standard LCD, and super LCD [17,18]. We have continued the proposal of Meal Tolerance Test (MTT). We always give diabetic two kinds of nutritional treatment which are CRD and LCD together. In similar way of Insulinogenic Index (IGI) for 75 g Oral Glucose Tolerance Test (OGTT), 70 g of carbohydrate in CRD can be enough applied for the study of the delta ratio of insulin/glucose at 0-30 min [19].
Furthermore, daily profile of blood glucose has been studied for CRD and LCD meals. These data were transformed into M value that is a numerical value indicating both of average blood glucose and Mean Amplitude Of Glycemic Excursions (MAGE). Both factors always influence blood glucose variability in the diabetic patients.
Combining the both research mentioned above together, authors have studied the pathophysiology of patients with SPIDDM and T2DM groups. In this study, we report the glucose variability of SPIDDM and the compare several biomarkers in the both groups.
Materials and Methods
In this study subjects enrolled were 24 patients with T2DM. They were recently diagnosed for T2DM, and admitted to the hospital. This is called as educational diabetic admission for 14 days, including the evaluation and treatment for diabetes.
Group 1 and 2
There are two groups of the subjects. Group 1 includes the patient diagnosed as T2DM in addition to the positive result for GADA. The presence of GADA would indicate the possibility of SPIDDM. There were 12 patients which were categorized into Group 1 (Table 1).
| Group | |||
| Caluculation of the average | mean ± SD | Median (25%-75%) | |
| Subjects | |||
| Group | |||
| Number | 12 | 12 | |
| Sex (male/female) | 4/8 | 4/8 | |
| Age (years old) | 54.9 ± 14.3 | 52.5 (46-63) | |
| Glucose | |||
| HbA1c (%) | 7.1 ± 0.9 | 7.3 (6.3-7.8) | |
| Glucose (0 min) mg/dL | 147 ± 46.4 | 150 (105-178) | |
| Glucose (30 min) mg/dL | 187 ± 66.9 | 169 (131-237) | |
| Antibody | |||
| Anti-GAD-Ab (U/mL) | 111 ± 134 | 76.4 (60.4-102) | |
| Intervention | Average Glucose (day 2) mg/dL) | 194 ± 59.1 | 187 (157-255) |
| Average Glucose (day 4) (mag/dL) | 147 ± 46.4 | 145 (114-172) | |
| M value (day 2) | 153 ± 148 | 76.5 (45.9-278) | |
| M value (day 4) | 63.8 ± 74.5 | 27.2 (19.3-83.5) |
Table 1 Basal data of the subjects with positive GAD-Ab.
On the other hand, group 2 has 12 patients with T2DM. Authors have a long experience of clinical practice and research for lots of diabetic patients who received the same protocol examination of the admission and investigation for 14 days. From many patients, 12 patients were picked up who showed the similar result of age, sex, HbA1c and average blood glucose to those of 12 patients in group 1. In other words, age, sex and data-matched 12 patients were recruited for group 2. The outlines of group 1 and 2 were shown in Table 2.
| Group | Group 1 | Group 2 | |
| GAD (+) | GAD (-) | ||
| Subjects | |||
| number | 12 | 12 | |
| sex (male/female) | 4/8 | 4/8 | |
| age (years old\imean+SD) | 54.9 ± 14.3 | 55.3 ± 15.7 | |
| (median (25%-75%)) | 52.5 (46-69) | 51.5 (43.5-69) | |
| M value (day 2) (mean ± SD) | 153 ± 148 | 123 ± 136 | |
| (median (25% - 75%)) | 76.9(45.9-278) | 69.9 (37.8-149) | |
| M value (day 4) (mean ± SD) | 63.8 ± 74.5 | 11.1 ± 11.8 | |
| (median (25% - 75%)) | 27.2(19.3-83.5) | 5.8 (3.5-13.3) |
Table 2 Comparision of glucose variability in 2 groups by GAD-Ab.
Basal data
Each patient was admitted to the hospital. In the morning on the next day after overnight fasting, blood samples were drawn for the examination of basal biochemistry. They included Complete Blood Count (CBC), liver and renal function test, blood lipids such as triglyceride, HDL-C, LDL-C and so on. As for the fundamental diabetic tests, preprandial and postprandial blood glucose, HbA1c, Immuno Reactivity of Insulin (IRI), C-peptide, Homeostasis Model Assessment of Insulin Resistance (HOMA-R), Homeostatic Model Assessment Beta cell function (HOMA-β), M value, GADA were measured for the basal data. The laboratory measurement method for GADA was Enzyme Immuno-Assay (EIA) (bridge method), in which the standard value is less than 5 U/mL.
CRD and LCD
The detail of the evaluation include several kinds of examination. They include i) To investigate the diabetic situation, ii) To study the daily profile of blood glucose, iii) To apply two patterns of diet therapy including CRD and LCD, iv) to check the responses of blood glucose and insulin secretion against the loading of breakfast including 70 g of carbohydrate, v) To compare the glucose variability by the calculation of the M value that indicates the mean level of average blood glucose in a day and MAGE.
Nutritional elements
Authors have continued clinical diabetic research using a certain protocol. It has two kinds of diet, which are CRD and LCD. CRD has given to the patients on day 1 and 2, which PFC ratio is 15: 25: 60 with 1400 kcal a day. This meal is the traditional Japanese meal pattern that was recommended as a standard diet from the Japan Diabetes Association (JDA) [20]. On the other hand, LCD was given to the patients from day 3 to day 14. We have three kinds of LCD, which are super-LCD, standard LCD, petite LCD, including the carbohydrate ratio as 12%, 26%, 40%, respectively. In our protocol, we applied super LCD with 1400 kcal/day providing from day 3 to day 14.
Lipids profile
In our protocol, lipids profiles such as triglyceride, HDL-C and LDL-C were measured on day 2 and day 14. The blood samples were withdrawn after overnight fasting. The data were compared in order to investigate the effect of the meal of LCD for 12 days.
Daily profile of glucose
The patients were studied for their daily profile of blood glucose. For the measurement of blood glucose, 7 times check per day was done, which were 08, 10, 12, 14, 17, 19 and 22 hour. Daily profile of glucose was investigated on day 2 and day 4. As to related nutritional therapy, meal on CR was served on day 1 and 2, and meal on LCD was served from day 3-14. Then, the difference between day 2 and day 4 means the short beneficial effect of LCD for only 2 days. After measuring blood glucose 7 times a day, the data was calculated into M value using the calculation equation of the formula about M value [21,22].
M value
As one of the evaluation method for glucose variability, M value has been known and applied for useful biomarker. The meaning of M value have two aspects. One is the level of the average blood glucose a day and another is the changing width of the glucose swinging. The latter has been called the MAGE [21-23]. Both are important markers which give various hyperglycemic influence for diabetic patients.
Consequently, M value is shown as one numerical value which means both levels of average glucose an MAGE. From the mathematic way of calculation, M value has been indicated as the equation of the logarithmic transformation. The medical significance of M value in the clinical practice would be that it can reveal the degree how far the glucose deviation is situated from the ideal daily glucose profile in a day [22-24].
The actual calculation method of M value has three steps. At first, there is a the basal equation, indicating M=MBS + MW. Then M value shows the total value of MBS and MW. Secondly, MW means the degree of fluctuation, by the calculation of (maximum blood glucose−minimum glucose)/20. Thirdly, MBS shows the mean level of MBSBS. When combining these three steps together, MBSBS means the individual M-value, that is calculated as (absolute value of [10×log (blood glucose level/ 120)])3 [22-24].
There is clinically standard evaluation way for M value, for the deviated glucose variability. As to the obtained results M value, the standard normal range is <180, borderline range is 180 and between 180 and 320, and abnormal range is 320 and more than 320.
Statistical analysis
Obtained data in current study were revealed by mean and standard deviation. In the case of some biomarkers, the results were revealed by the average in median and the quartile values of 25% and 75%. There are some biomarkers which are described as the median and quartiles of 25% and 75%. When evaluating the correlation among biomarkers, the Spearman test was applied for the correlation coefficients in the analyses. Furthermore, the computerized standard statistical tool has been used for analyzing some statistical evaluation [25].
Ethical Consideration
Current study was fundamentally performed in compliance with the ethical principles on the Declaration of Helsinki. Further, additional commentary was conducted on the Ethical Guidelines for Research in the medical field for Humans and in accordance with the Good Clinical Practice (GCP). Those were found associated with the ongoing consideration for the protection of human rights. In addition, “Ethical Guidelines for Epidemiology Research” was applied as an adequate guideline. This was presented in Japan by the Ministry of Education, Culture, Sports, Science and Technology and the Ministry of Health, Labor and Welfare.
Author’s have established an ethical committee. Regarding the discussion on the medical and ethical problems, professions were medical doctor, nurse, pharmacist, nutritionist and other experts in the legal specialty. As regard to the study, our discussion has become appropriate and valid, with the agreements. In the light of patient standpoint, the informed consents and written document agreements have been taken from all subjects. This study has been registered by National University Hospital Council of Japan (ID: #R000031211).
Results
Fundamental data
In this study, 12 patients with T2DM were enrolled with positive result for GADA. Their basal data were shown in Table 1. Their data were described by mean ± SD, and median/quartile of 25%/75%. Average ages was 54.9 ± 14.3 years old. Average HbA1c was 7.1 ± 0.9%, and median HbA1c value was 7.3%. On the morning of day 2, patient had breakfast of CRD with 70 g of carbohydrate. The levels of blood glucose of 0 min and 30 min was 147 mg/dL and 187 mg/dL, respectively. The result of GADA (U/mL) was 76.4 (60.4-102) (median (25%-75%)).
Daily profile of blood glucose
Average blood glucose in day 2 and day 4 was 194 ± 59.1 mg/dL and 147 ± 46.4 mg/dL, respectively (Table 1). Converting the data of daily profile of blood glucose into M value, the median level of M value in day 2 and day 4 was 76.9 and 27.2, respectively (Table 1).
Comparison of groups
According to the detail data of 12 subjects in group 1, adequate 12 subjects were enrolled for group 2 in the light of age, sex, HbA1c and average glucose. The data in group 1 and 2 were summarized and compared in Table 2. In both groups, there are similar results in age and M value on day 2. However, there is remarkable difference of M value on day 4 between group 1 and group 2 (Table 2).
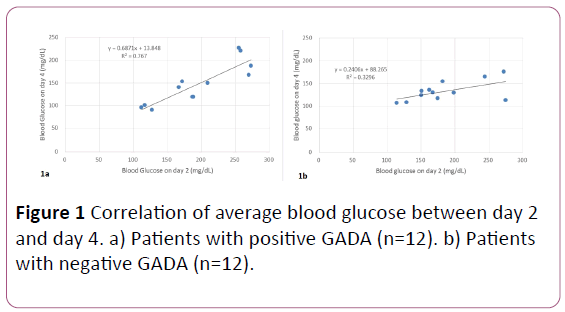
Decreased glucose
Average blood glucose was measured in day 2 and day 4, and the correlation between them is shown in Figure 1. In both group, average blood glucose on day 2 were in the same level. Average blood glucose on day 4 in group 1 was moderately decreased (Figure 1a). Its regression curve was y=0.68 x+13.8. On the other hand, average blood glucose on day 4 in group 2 was remarkably decreased (Figure 1). Its regression curve was y=0.24x+88.3. Consequently, there is difference of decreased blood value between group 1 and group 2.
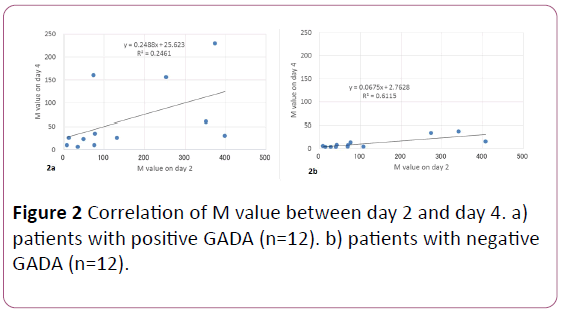
Decreased M value
M value was measured in day 2 and day 4, and the correlation between them is shown in Figure 2. In both group, M value on day 2 were in the same level. According to the data of M value on day 4 in group 1, 9 cases showed moderately decreased, but 3 cases showed not so decreased (Figure 1). Its regression curve was y=0.25x+25.6. In contrast, M value on day 4 in group 2 was remarkably decreased in all 12 cases (Figure 1). Its regression curve was y=0.07x+2.8. Consequently, there is large difference of M value between group 1 and group 2.
Discussion
According to the quartile analysis, 50% of the subjects in this study were 46-63 years of age, 6.3%-7.8% of HbA1c value. It seemed to be generally standard level and distribution. Subjects were given a standard breakfast of CRD containing 70 g of carbohydrate on the morning in day 2 [19]. This is one of the MTT, and it induced increased blood glucose and insulin secretion, which were sufficient responses in the light of clinical study.
For MTT, a breakfast of 450 kcal was initially attempted as a test meal. The ratio of the nutrients was PFC=15:35:50, and the amount of carbohydrate was 56 g [26]. After that, a trial of highprotein Boost-HP formula meal was made. It included 33 g of carbohydrate, 15 g of protein and 6 g of fat [27].
As a standard test, 75 g of OGTT has been applied in the clinical practice using 75 g of carbohydrate. Similarly, we have continued MTT utilizing a breakfast containing 70 g of carbohydrate as a standard diet by CRD [19]. In addition to blood glucose, IRI and/or C-peptide against 70 g of carbohydrate have been also examined. Clinically, IGI-carbo 70 has been proposed and can be used in the clinical practice of diabetes in the future.
Among several biomarkers, GADA, M value (day 2) and M value (day 4) showed larger standard deviation value compared with the average value of the mean. In these factors, median value and quartile values of 25%/75% would be beneficial and useful for obtaining the general situation [28]. One of the reason would be the logarithmic distribution of the data from these factors.
Enrolled 12 subjects with positive GADA (group 1) and datamatched 12 subjects with T2DM (group 2) are compared. Both groups showed almost the same age, sex, blood glucose and M value on day 2. However, M value on day 4 showed remarkable difference between both groups. This result suggest that the insulin secretion in group 1 may show less glucose-lowering effect in response to LCD meal.
There were significant correlation of blood glucose between day 2 and day 4, in group 1 (GADA positive) and group 2 (GADA negative). The values of glucose on day 2 were almost the same in both group. However, the values of glucose on day 4 were higher in group 1.
According to the regression curves of both group, three glucose value can be input as 150 mg/dL, 200 mg/dL, 250 mg/dL as day 2. Estimated glucose on day 4 in group 1 vs group 2 would be 117 mg/dL vs 124 mg/dL, 152 mg/dL vs 136 mg/dL and 186 mg/dL vs 148 mg/dL, respectively. Thus, glucose value was higher in group 1 (GADA positive) than that in group 2 (GADA negative).
Similar to average blood glucose, M value on day 2 showed almost the same level in both groups. However, M value on day 4 in group 1 did not decrease so much as that in group 2. Regarding the correlation of M value between day 2 and day, the distribution was wider in group 1, and it was narrower in group 2. These results suggest that patients in group 1 would show various responses for LCD intervention, and patients in group 2 would show satisfactory similar responses for LCD intervention with narrow distribution.
Comparing the both correlation of average blood glucose and M value, detail difference of glucose variability can be found in M value study rather than glucose study [24]. It is due to the characteristic point that M value reflects average blood glucose and MAGE. Consequently, current study method including daily profile of blood glucose, average glucose and M value can be useful for investigating not only present glucose variability, but also future prediction for insulin secretion or diabetic status.
As regard to T1DM and SPIDDM, there have been some Diabetes-Associated Autoantibody (DAA) in the light of immunological aspect. Most sensitive marker is GADA in T1DM and SPIDDM [29,30]. In the case of younger patients with recent diagnosis of T1DM, rather frequent antibodies are Insulin Auto- Antibodies (IAA), protein tyrosine phosphatase IA-2 (IA-2A), and islet-specific zinc transporter isoform 8 (ZnT8). In contrast, there are rather less found for SPIDDM [30].
From the former medical reports, the prevalence for GADA in normal population was about 0.5% – 0.8% [31]. In reference, T2DM without insulin therapy was 2%-6%, and T2DM with insulin dependent situation later was 11%–15%. Due to these data, GADA could be responsible for the onset of diabetes and decreased function of insulin secretion [32,33].
SPIDDM has been believed to be from the destruction of betacell by islet-cell autoimmunity, and it is gradually proceeded to the level of an insulin-dependent situation for long years [34]. The evidence of GADA has been necessary for diagnosis of SPIDDM, but there were some controversy about the GADA assay method by Radioimmunoassay (RIA) or Enzyme-Linked Immunosorbent Assay (ELISA) [34].
Several reports are found about the measurement system for GADA [35]. There was actually GADA-RIA way applied for clinical practice. If the results of the titers level were classified into high group and low group, C-peptide value was 0.73 ng/mL and 0.68 ng/mL, respectively without significance [35]. In contrast, if the results measured by GADA-ELISA were classified between positive and negative, C-peptide value was 0.85 ng/mL and 2.60 ng/mL, respectively with significant difference. Consequently, GADA-ELISA seems to be beneficial for suggesting decreased ability of insulin secretion [35].
What is the detail pathophysiology of SPIDDM? Endogenous insulin secretion is maintained in T2DM but it is almost abolished in T1DM. Actually, however, slight insulin secretion is observed in T1DM as measured by the ultrasensitive C-peptide assay [36]. Clinical study for T1DM patients with a long diabetes history revealed that endogenous insulin secretion was detected in 80% of cases [37]. Even with these clinical data, the details of sustained insulin secretion in T1DM are still unclarified [38]. Future development would be expected with the elucidation of the pathological condition of SPIDDM
There was a nationwide survey for SPIDDM in Japan. It is multi-center study for study genetic characteristics for SPIDDM by the Japan Diabetes Society (JDS) [9]. Patients with SPIDDM were classified into two groups, which are Non-Insulin-Requiring SPIDDM (NIR-SPIDDM) and Insulin-Requiring SPIDDM (IRSPIDDM). By comparing these two groups, NIR-SPIDDM revealed as follows: i) Later onset of diabetes, ii) Higher body mass index, iii) Longer history before diagnosis, iv) Rarer hyperglycemic symptoms at onset, v) Higher level of C-peptide, LDL-cholesterol and Triglyceride (TG) values compared to those of IR-SPIDDM. From genetic point of view, NIR-SPIDDM revealed vi) Less frequency of susceptible HLA-DRB1*04:05-DQB1*04:01 and vii) Higher frequency of resistant HLA-DRB1*15:01-DQB1*06:02 haplotype [9].
There is a limitation for this report. For T2DM cases with positive GADA, further evaluation of their background, other autoantibodies or related biomarkers, correlations among some biomarkers and so on would be required. More cases and detail analyses will be needed in the future.
Conclusion
In summary, 12 patients of T2DM with positive GADA (group 1) received diabetic evaluation such as daily profile of blood glucose for CRD and LCD, converted analysis of M value and correlations among related biomarkers. Further, compared with recruited 12 cases of T2DM with matching age and data (group 2), there are cases where the reduction of average blood glucose by LCD is insufficient in group 1, suggesting the possibility of progress to SPIDDM status. Further analyses would be continued and expected for future research in this field.
References
- Kamishima K, Ogawa H, Jujo K, Yamaguchi J, Hagiwara N (2019) Relationships between blood pressure lowering therapy and cardiovascular events in hypertensive patients with coronary artery disease and type 2 diabetes mellitus: The HIJ-CREATE sub-study. Diabetes Res Clin Pract 149: 69-77
- Davies MJ, D'Alessio DA, Fradkin J, Kernan WN, Mathieu C, et al. (2018) Management of Hyperglycemia in Type 2 Diabetes, 2018. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Carev 41: 2669-2701.
- American Diabetes Association (2014) Diagnosis and classification of diabetes mellitus. Diabetes Care 37: S81–S90.
- Mulukutla SN, Acevedo-Calado M, Hampe CS, Pietropaolo M, Balasubramanyam A (2018) Autoantibodies to the IA-2 Extracellular Domain Refine the Definition of “A+” Subtypes of Ketosis-Prone Diabetes. Diabetes Care 41: 2637-2640.
- Haneda M, Noda M, Origasa H, Noto H, Yabe D, et al. (2018) Japanese Clinical Practice Guideline for Diabetes 2016. J Diabetes Investig 9: 657–697.
- Kawasaki E, Maruyama T, Imagawa A (2013) Diagnostic criteria for acute-onset type 1 diabetes mellitus (2012): Report of the Committee of Japan Diabetes Society on the Research of Fulminant and Acute-onset Type 1 Diabetes Mellitus. Diabetol Int 4: 221.
- Tanaka S, Ohmori M, Awata T (2015) Diagnostic criteria for slowly progressive insulin-dependent (type 1) diabetes mellitus (SPIDDM) (2012): report by the Committee on Slowly Progressive Insulin-Dependent (Type 1) Diabetes Mellitus of the Japan Diabetes Society. Diabetol Int 6: 149.
- Kobayashi T, Nakanishi K, Murase T, Kosaka K (1996) Small doses of subcutaneous insulin as a strategy for preventing slowly progressive beta-cell failure in islet cell antibody-positive patients with clinical features of NIDDM. Diabetes 45: 622–626.
- Yasui J, Kawasaki E, Tanaka S, Awata T, Ikegami H, et al. (2016) Clinical and genetic characteristics of non-insulin-requiring glutamic acid decarboxylase (GAD) autoantibody-positive diabetes: a nationwide survey in Japan. PLoS One 11: e0155643
- Atkins RC (1981) Dr. Atkins’ diet revolution. Bantam Books, New York.
- Bernstein RK (1997) Dr. Bernstein's Diabetes Solution. Little, Brown and company, New York.
- Shai I, Schwarzfuchs D, Henkin Y, Shahar DR, Witkow S, et al. (2008) Weight Loss with a Low-Carbohydrate, Mediterranean, or Low-Fat Diet. N Engl J Med 359: 229-241.
- Schwarzfuchs D, Golan R, Shai I (2012) Four-year follow-up after two-year dietary interventions. N Engl J Med 367: 1373-1374.
- Meng Y, Bai H, Wang S, Li Z, Wang Q (2017) Efficacy of low carbohydrate diet for type 2 diabetes mellitus management: A systematic review and meta-analysis of randomized controlled trials. Diabetes Res Clin Pract 131:124-131.
- Churuangsuk C, Lean M, Combet E (2018). Low-carbohydrate diet score is associated with higher glycated haemoglobin: a secondary analysis of the UK national diet and nutrition surveys year 1–6. Clinical Nutrition 37: S304.
- Ebe K, Ebe Y, Yokota S, Matsumoto T, Hashimoto M, et al. (2004) Low Carbohydrate diet (LCD) treated for three cases as diabetic diet therapy. Kyoto Medical Association Journal 51: 125-129.
- Bando H, Ebe K, Muneta T, Bando M, Yonei Y (2017) Effect of low carbohydrate diet on type 2 diabetic patients and usefulness of M-value. Diabetes Res Open J 2017; 3: 9-16.
- Ebe K, Bando H, Yamamoto K, Bando M, Yonei Y (2018) Daily carbohydrate intake correlates with HbA1c in low carbohydrate diet (LCD). J Diabetol 1: 4-9.
- Bando H, Ebe K, Muneta T, Bando M, Yonei Y (2017) Proposal for Insulinogenic Index (IGI)-Carbo70 as Experimental Evaluation for Diabetes. J Clin Exp Endocrinol 1: 102.
- Japan Diabetes Association (2013) Diabetes clinical practice guidelines Based on scientific evidence.
- Schlichtkrull J, Munck O, Jersild M (1965) The M-value, an index of blood sugar control in diabetics. Acta Med Scand 177: 95–102.
- Service FJ, Molnar GD, Rosevear JW, Ackerman E, Gatewood LC, et al. (1970) Mean amplitude of glycemic excursions, a measure of diabetic instability. Diabetes 19: 644-655.
- Molnar GD, Taylor WF, Ho MM (1972) Day-to-day variation of continuously monitored glycaemia: A further measure of diabetic instability. Diabetologia 8: 342-348.
- Moberg E, Kollind M, Lins PE, Adamson U (1993) Estimation of blood-glucose variability in patients with insulin-dependent diabetes mellitus. Scand J Clin Lab Invest 53: 507-514.
- Yanai H (2015) Four step excel statistics, 4th Edition, Seiun-sha Publishing Co.Ltd, Tokyo.
- Yoshino G, Tominaga M, Hirano T, Shiba T, Kashiwagi A, et al. (2006) The test meal A:A pilot model for the international standard of test meal for an assessment of both postprandial hyperglycemia and hyperlipidemia. J Jpn Diabetes Soc 49:361–371.
- Bacha F, Gungor N, Lee S, de las Heras J, Arslanian S (2013) Indices of insulin secretion during a liquid mixed-meal test in obese youth with diabetes. J Pediatr 162(5):924-9.
- Walston CE, Felix CP (1977) A method of programming measurement and estimation. IBM Systems Journal 16: 54-73.
- Hawa MI, Kolb H, Schloot N, Beyan H, Paschou SA, et al. Action LADA consortium (2013) Adult-onset autoimmune diabetes in Europe is prevalent with a broad clinical phenotype: Action LADA 7. Diabetes Care 36: 908-913.
- Lampasona V, Petrone A, Tiberti C, Capizzi M, Spoletini M, et al. (2010) Non Insulin Requiring Autoimmune Diabetes (NIRAD) Study Group. (2010) Zinc transporter 8 antibodies complement GAD and IA-2 antibodies in the identification and characterization of adult-onset autoimmune diabetes: Non Insulin Requiring Autoimmune Diabetes (NIRAD) 4. Diabetes Care 33: 104-108.
- Takeda H, Kawasaki E, Shimizu I, Konoue E, Fujiyama M, et al. (2002) Clinical, autoimmune, and genetic characteristics of adult-onset diabetic patients with GAD autoantibodies in Japan (Ehime Study). Diabetes Care 25: 995–1001.
- Tanaka S, Okubo M, Nagasawa K, Takizawa S, Ichijo M, et al. (2015) Predictive value of titer of GAD antibodies for further progression of beta cell dysfunction in slowly progressive insulin-dependent (type 1) diabetes (SPIDDM). Diabetology International 7: 42-52.
- Takeuchi Y, Ito H, Oshikiri K, Antoku S, Abe M, et al. (2012) Reduced endogenous insulin secretion in diabetic patients with low-titer positive antibodies against GAD. J Diabetes Mellitus 2: 96-100.
- Oikawa Y, Tanaka H, Uchida J, Atsumi Y, Osawa M, et al. (2017) Slowly progressive insulin-dependent (type 1) diabetes positive for anti-GAD antibody ELISA test may be strongly associated with a future insulin-dependent state. Endocr J 64: 163-170.
- Oikawa Y Katsuki T, Kawai T, Shimada A (2018) A Cut-Off Value for Anti-GAD Ab ELISA Test for Predicting Future Insulin Dependency in SPIDDM May Not Exist. Diabetes 67(Supp 1).
- Davis AK, DuBose SN, Haller MJ, Miller KM, DiMeglio LA, Network TDEC, et al. (2015) Prevalence of detectable C-Peptide according to age at diagnosis and duration of type 1 diabetes. Diabetes Care 38: 476-481
- Oram RA, McDonald TJ, Shields BM, Hudson MM, Shepherd MH, et al. (2015) Team U (2015) Most people with long-duration type 1 diabetes in a large population-based study are insulin microsecretors. Diabetes Care 38: 323-328
- Pietropaolo M (2013) Persistent C-peptide: what does it mean? Current Opinion in Endocrinology, Diabetes and Obesity 20: 279-284

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences